A tracheostomy is a medical procedure that creates an opening in the neck to access the trachea, allowing for enhanced breathing and airway management. It is commonly performed for patients requiring long-term ventilation or those with obstructed airways. Explore this article to understand the procedure, risks, and care required for a tracheostomy.
Table of Comparison
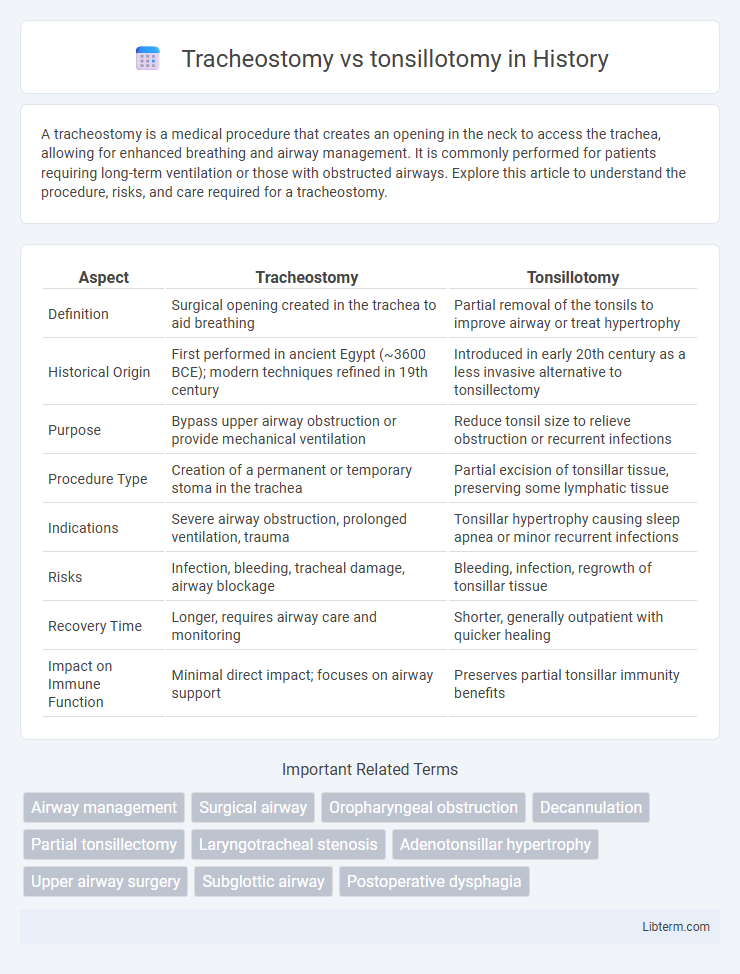
| Aspect | Tracheostomy | Tonsillotomy |
|---|---|---|
| Definition | Surgical opening created in the trachea to aid breathing | Partial removal of the tonsils to improve airway or treat hypertrophy |
| Historical Origin | First performed in ancient Egypt (~3600 BCE); modern techniques refined in 19th century | Introduced in early 20th century as a less invasive alternative to tonsillectomy |
| Purpose | Bypass upper airway obstruction or provide mechanical ventilation | Reduce tonsil size to relieve obstruction or recurrent infections |
| Procedure Type | Creation of a permanent or temporary stoma in the trachea | Partial excision of tonsillar tissue, preserving some lymphatic tissue |
| Indications | Severe airway obstruction, prolonged ventilation, trauma | Tonsillar hypertrophy causing sleep apnea or minor recurrent infections |
| Risks | Infection, bleeding, tracheal damage, airway blockage | Bleeding, infection, regrowth of tonsillar tissue |
| Recovery Time | Longer, requires airway care and monitoring | Shorter, generally outpatient with quicker healing |
| Impact on Immune Function | Minimal direct impact; focuses on airway support | Preserves partial tonsillar immunity benefits |
Introduction to Tracheostomy and Tonsillotomy
Tracheostomy is a surgical procedure that creates an opening through the neck into the trachea to establish an airway for patients with respiratory obstruction or failure. Tonsillotomy involves partial removal of the palatine tonsils to relieve chronic tonsillar hypertrophy or obstruction while preserving immune function. Both procedures address airway management but target different anatomical sites and indications.
Indications for Tracheostomy
Tracheostomy is primarily indicated for airway obstruction due to tumors, trauma, or prolonged intubation, ensuring a secure airway when upper airway patency is compromised. It is also performed in cases of severe sleep apnea, respiratory failure, or neuromuscular diseases that impair breathing. In contrast, tonsillotomy is typically indicated for partial removal of hypertrophic tonsils causing obstructive sleep apnea or recurrent tonsillitis, mainly addressing localized tonsillar issues without affecting airway access.
Indications for Tonsillotomy
Tonsillotomy is primarily indicated for patients with obstructive sleep apnea, recurrent tonsillitis, or tonsillar hypertrophy causing airway obstruction. Unlike tracheostomy, which is reserved for severe airway obstruction or prolonged ventilation needs, tonsillotomy offers a less invasive solution to improve airway patency and reduce infection frequency. This procedure preserves the tonsillar capsule, resulting in faster recovery and fewer complications compared to tonsillectomy.
Surgical Procedures Overview
Tracheostomy involves creating a direct airway through an incision in the trachea to bypass upper airway obstructions, typically performed under general anesthesia with precise incision and tube placement techniques. Tonsillotomy, a partial removal of the tonsils, is conducted using methods such as cold steel dissection or electrocautery to reduce tonsillar tissue while preserving the capsule, often for treating obstructive sleep apnea or recurrent infections. Both procedures require careful patient assessment, sterile surgical environments, and post-operative monitoring to minimize complications and ensure airway patency or reduced tonsillar hypertrophy.
Risks and Complications Comparison
Tracheostomy carries risks such as bleeding, infection, tracheal stenosis, and accidental decannulation, which can lead to airway obstruction and respiratory distress. Tonsillotomy, being less invasive, typically presents fewer severe complications but may cause postoperative bleeding, pain, and, rarely, airway obstruction due to swelling. Comparing both, tracheostomy complications are more critical due to direct airway involvement, while tonsillotomy risks are generally limited to local tissue response and hemorrhage.
Recovery and Post-Operative Care
Recovery after tracheostomy generally involves longer hospital stays due to airway management and potential complications such as infection or bleeding, requiring intensive post-operative care including suctioning, humidification, and regular stoma cleaning. Tonsillotomy typically allows for faster recovery with less pain, shorter hospitalization, and fewer dietary restrictions, emphasizing pain control, hydration, and monitoring for bleeding as key components of post-operative care. Both procedures necessitate vigilant observation for respiratory status changes, but tracheostomy demands more specialized nursing intervention and patient education to manage the airway tube effectively.
Long-Term Outcomes
Tracheostomy provides long-term airway management and is associated with improved respiratory function and reduced risk of airway obstruction in patients requiring prolonged ventilation. Tonsillotomy, a less invasive alternative to tonsillectomy, offers quicker recovery and lower postoperative pain but may have a higher recurrence rate of tonsillar hypertrophy compared to complete tonsil removal. Long-term outcomes favor tracheostomy for chronic airway support, whereas tonsillotomy is preferred for cases needing partial tonsil tissue reduction with minimized surgical trauma.
Pediatric vs Adult Considerations
Tracheostomy in pediatric patients requires careful consideration due to smaller airway anatomy and higher risk of complications such as granulation tissue and accidental decannulation, whereas adults typically have more stable airway structures but face higher risks of infection and long-term tracheal stenosis. Tonsillotomy, often preferred in children to reduce postoperative pain and bleeding compared to tonsillectomy, is less commonly performed in adults, where tonsillectomy remains the standard due to the prevalence of recurrent infections or malignancy concerns. Pediatric airway management emphasizes growth and development factors, while adult treatment prioritizes comorbidities and airway rigidity in choosing between tracheostomy and tonsillotomy.
Cost and Resource Implications
Tracheostomy procedures typically incur higher costs due to the need for specialized surgical equipment, longer hospital stays, and intensive postoperative care compared to tonsillotomy. Tonsillotomy generally requires fewer resources, shorter anesthesia time, and faster patient recovery, resulting in lower overall healthcare expenses. The choice between the two affects resource allocation significantly, with tracheostomy often demanding more extensive staffing and facility support.
Choosing the Appropriate Procedure
Choosing the appropriate procedure between tracheostomy and tonsillotomy depends on the patient's airway obstruction severity and underlying condition. Tracheostomy is typically indicated for long-term airway management in cases of severe upper airway obstruction, prolonged ventilation, or chronic respiratory failure. Tonsillotomy is preferred for less invasive treatment of obstructive tonsillar hypertrophy causing sleep apnea or recurrent infections, offering faster recovery and fewer complications.
Tracheostomy Infographic
 libterm.com
libterm.com