Coagulation is the process by which blood changes from a liquid to a gel, forming a clot to stop bleeding and initiate healing. This essential mechanism involves platelets and clotting factors working together to seal damaged blood vessels and prevent excessive blood loss. Discover how this critical biological function protects your body and what factors can influence its efficiency in the rest of the article.
Table of Comparison
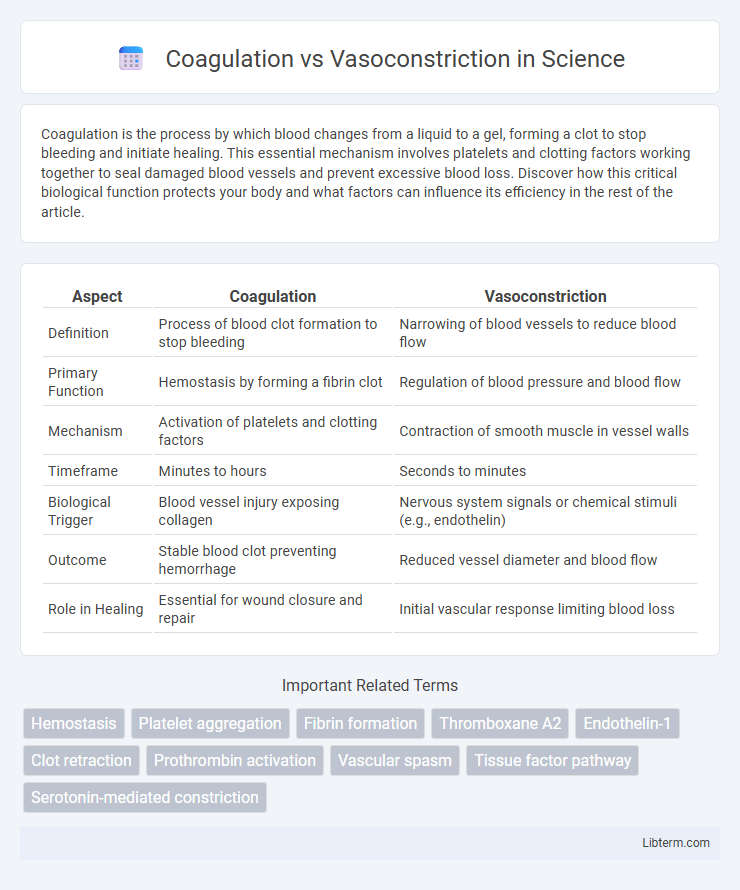
| Aspect | Coagulation | Vasoconstriction |
|---|---|---|
| Definition | Process of blood clot formation to stop bleeding | Narrowing of blood vessels to reduce blood flow |
| Primary Function | Hemostasis by forming a fibrin clot | Regulation of blood pressure and blood flow |
| Mechanism | Activation of platelets and clotting factors | Contraction of smooth muscle in vessel walls |
| Timeframe | Minutes to hours | Seconds to minutes |
| Biological Trigger | Blood vessel injury exposing collagen | Nervous system signals or chemical stimuli (e.g., endothelin) |
| Outcome | Stable blood clot preventing hemorrhage | Reduced vessel diameter and blood flow |
| Role in Healing | Essential for wound closure and repair | Initial vascular response limiting blood loss |
Understanding Hemostasis: Coagulation and Vasoconstriction
Coagulation involves the formation of a fibrin mesh through a complex cascade of platelet activation and clotting factors to prevent blood loss after vascular injury. Vasoconstriction is the immediate narrowing of blood vessels triggered by smooth muscle contraction to reduce blood flow and limit hemorrhage. Both processes are essential for effective hemostasis, working synergistically to stabilize the wound site and initiate tissue repair.
Defining Coagulation: Process and Key Players
Coagulation is the complex biological process where blood transforms from a liquid to a gel, preventing excessive bleeding by forming a stable clot. Key players include platelets, which aggregate at injury sites, and clotting factors such as fibrinogen, thrombin, and Factor VIII that interact in a cascade to produce fibrin strands. This tightly regulated mechanism complements vasoconstriction, the initial narrowing of blood vessels that reduces blood flow and supports clot formation.
Vasoconstriction: Definition and Mechanisms
Vasoconstriction is the narrowing of blood vessels resulting from the contraction of muscular walls, primarily in the arteries and arterioles. This physiological process reduces blood flow and increases vascular resistance, playing a critical role in regulating blood pressure and minimizing blood loss after vascular injury. Mechanisms of vasoconstriction involve autonomic nervous system activation, particularly the release of norepinephrine, and the action of vasoactive substances such as endothelin and angiotensin II on smooth muscle cells.
Biological Purpose: Why Coagulation and Vasoconstriction Occur
Coagulation and vasoconstriction are vital biological processes that work together to prevent excessive blood loss after vascular injury. Vasoconstriction narrows blood vessels, reducing blood flow to the damaged area and minimizing hemorrhage, while coagulation involves a complex cascade of clotting factors that form a stable fibrin clot to seal the vascular breach. These mechanisms ensure hemostasis by rapidly stabilizing blood loss and initiating tissue repair.
Molecular Pathways: Coagulation Cascade vs Vasoconstriction Pathways
The coagulation cascade involves a series of proteolytic activations of clotting factors, primarily in the intrinsic, extrinsic, and common pathways, leading to the conversion of fibrinogen into fibrin to stabilize the blood clot. Vasoconstriction pathways are driven by molecular signals such as endothelin-1, angiotensin II, and increased intracellular calcium in smooth muscle cells, resulting in vessel lumen narrowing. While coagulation focuses on enzymatic reactions for clot formation, vasoconstriction modulates vascular tone through receptor-mediated smooth muscle contraction.
Role in Wound Healing: Coagulation vs Vasoconstriction
Coagulation plays a critical role in wound healing by forming a stable blood clot that prevents excessive blood loss and provides a scaffold for tissue repair. Vasoconstriction, triggered immediately after injury, reduces blood flow to the damaged area to minimize bleeding and facilitate clot formation. Together, these processes are essential for hemostasis, initiating the cascade that leads to tissue regeneration and wound closure.
Key Differences: Coagulation vs Vasoconstriction
Coagulation is the process by which blood transforms from a liquid to a gel, forming clots that prevent excessive bleeding by stabilizing injured blood vessels. Vasoconstriction refers to the narrowing of blood vessels caused by the contraction of muscular walls, reducing blood flow to minimize blood loss and facilitate clot formation. While coagulation primarily involves platelet aggregation and fibrin meshwork, vasoconstriction is a rapid, neural or hormonal response that decreases vessel diameter to limit hemorrhage.
Clinical Significance: Disorders of Coagulation and Vasoconstriction
Disorders of coagulation include hemophilia and deep vein thrombosis, where impaired clot formation or excessive clotting leads to bleeding or thrombosis, respectively. Vasoconstriction abnormalities contribute to conditions such as hypertension and Raynaud's phenomenon by causing excessive narrowing of blood vessels, resulting in reduced blood flow and tissue ischemia. Clinical management often requires targeted therapies to either promote hemostasis in coagulation disorders or relax vascular smooth muscle in vasoconstriction-related diseases.
Diagnostic Approaches: Assessing Hemostatic Disorders
Diagnostic approaches for assessing hemostatic disorders differentiate between coagulation and vasoconstriction by utilizing specific tests such as platelet function assays, bleeding time evaluation, and coagulation factor analysis. Laboratory techniques like thromboelastography (TEG) and platelet aggregometry effectively measure clot formation dynamics and vasoconstrictive platelet activity, aiding in precise identification of underlying pathologies. Advanced imaging and biochemical markers complement these tests, enhancing diagnostic accuracy for conditions like von Willebrand disease, thrombocytopenia, and vascular abnormalities affecting hemostasis.
Therapeutic Interventions: Managing Coagulation and Vasoconstriction Disorders
Therapeutic interventions for managing coagulation disorders include anticoagulants such as warfarin, heparin, and direct oral anticoagulants (DOACs) to prevent thrombus formation and reduce the risk of stroke or deep vein thrombosis. Vasoconstriction disorders are treated with vasodilators like calcium channel blockers and ACE inhibitors that improve blood flow by relaxing vascular smooth muscles and lowering blood pressure. Targeted therapies aim to balance coagulation and vasomotor tone, minimizing complications from excessive clotting or abnormal vessel constriction.
Coagulation Infographic
 libterm.com
libterm.com