Hemostasis is the body's natural process to prevent excessive bleeding by forming blood clots at injury sites. This crucial mechanism involves vascular constriction, platelet activation, and the coagulation cascade working together to restore vascular integrity. Explore the rest of the article to understand how hemostasis protects your body and influences medical treatments.
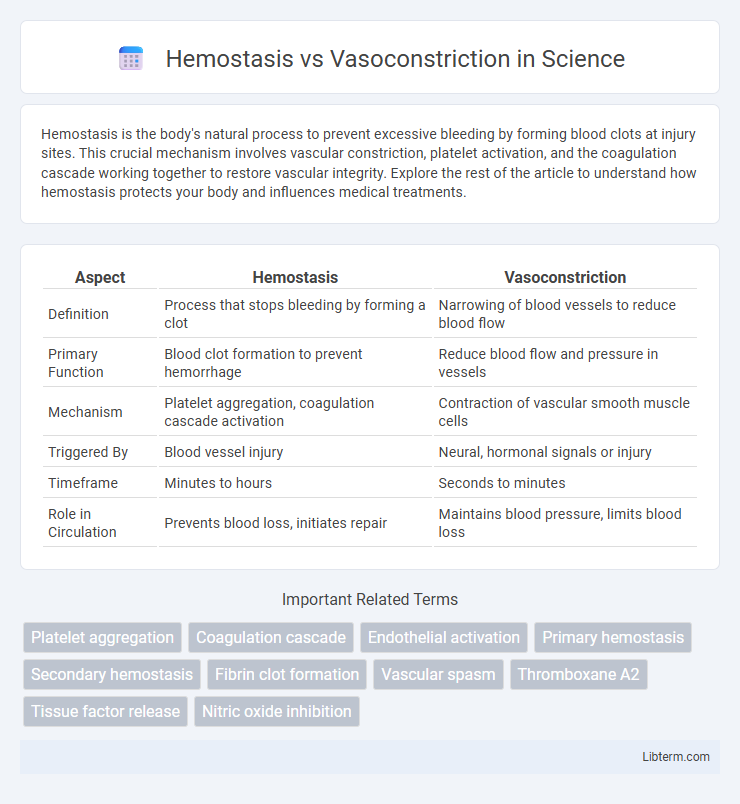
Table of Comparison
| Aspect | Hemostasis | Vasoconstriction |
|---|---|---|
| Definition | Process that stops bleeding by forming a clot | Narrowing of blood vessels to reduce blood flow |
| Primary Function | Blood clot formation to prevent hemorrhage | Reduce blood flow and pressure in vessels |
| Mechanism | Platelet aggregation, coagulation cascade activation | Contraction of vascular smooth muscle cells |
| Triggered By | Blood vessel injury | Neural, hormonal signals or injury |
| Timeframe | Minutes to hours | Seconds to minutes |
| Role in Circulation | Prevents blood loss, initiates repair | Maintains blood pressure, limits blood loss |
Introduction to Hemostasis and Vasoconstriction
Hemostasis is the physiological process that stops bleeding by forming a blood clot through vascular constriction, platelet aggregation, and coagulation cascades. Vasoconstriction refers specifically to the narrowing of blood vessels caused by contraction of the muscular wall, which reduces blood flow and minimizes blood loss. Both mechanisms work in tandem to maintain vascular integrity and prevent hemorrhage following vascular injury.
Definitions: Hemostasis vs Vasoconstriction
Hemostasis is the physiological process that stops bleeding by forming a stable blood clot through vascular constriction, platelet aggregation, and coagulation cascade activation. Vasoconstriction specifically refers to the narrowing of blood vessels caused by the contraction of vascular smooth muscle, reducing blood flow to minimize blood loss. While vasoconstriction is an initial step in hemostasis, hemostasis encompasses a broader range of mechanisms including platelet plug formation and fibrin clot stabilization.
The Role of Hemostasis in Bleeding Control
Hemostasis is crucial for bleeding control as it rapidly forms a temporary plug at the injury site through platelet aggregation and activation of the coagulation cascade. This process stabilizes the damaged blood vessel and prevents excessive blood loss by promoting fibrin clot formation. Vasoconstriction complements hemostasis by narrowing blood vessels, which reduces blood flow and supports clot stabilization during the initial response to vascular injury.
Mechanisms and Phases of Hemostasis
Hemostasis involves three primary phases: vascular spasm, platelet plug formation, and coagulation, aimed at stopping bleeding by forming a stable blood clot. Vasoconstriction is the initial mechanism during the vascular spasm phase, where blood vessels constrict to reduce blood flow and limit blood loss at the injury site. Platelets aggregate to form a temporary plug, followed by the coagulation cascade that stabilizes the plug with fibrin to achieve effective hemostasis.
Understanding Vasoconstriction in Blood Vessel Regulation
Vasoconstriction involves the narrowing of blood vessels through the contraction of vascular smooth muscle cells, which reduces blood flow and increases blood pressure, playing a critical role in blood vessel regulation. Unlike hemostasis, which encompasses the entire process of stopping bleeding including platelet aggregation and clot formation, vasoconstriction primarily provides an immediate response to vascular injury by minimizing blood loss. This mechanism is essential in maintaining vascular tone and regulating systemic blood pressure, directly impacting tissue perfusion and cardiovascular stability.
Triggers and Biochemical Pathways of Vasoconstriction
Vasoconstriction is triggered primarily by vascular injury, sympathetic nervous system activation, and local chemical signals such as endothelin and thromboxane A2, which initiate smooth muscle contraction in blood vessel walls. The biochemical pathways involve the release of calcium ions (Ca2+) within vascular smooth muscle cells, activating myosin light-chain kinase (MLCK) that phosphorylates myosin to induce contraction, alongside the involvement of vasoconstrictors like angiotensin II and norepinephrine binding to G-protein coupled receptors (GPCRs). These mechanisms contrast with hemostasis, where platelet aggregation and coagulation cascades work to form a stable blood clot to stop bleeding.
Key Differences Between Hemostasis and Vasoconstriction
Hemostasis is a complex physiological process that stops bleeding through blood clot formation involving platelets and coagulation factors, whereas vasoconstriction is the narrowing of blood vessels caused by smooth muscle contraction to reduce blood flow. Hemostasis includes platelet plug formation and fibrin clot stabilization, while vasoconstriction primarily manages blood flow and pressure at the injury site. The key difference lies in hemostasis achieving hemostatic wound closure, whereas vasoconstriction serves as an immediate vascular response to minimize blood loss.
Clinical Significance: Hemostasis vs Vasoconstriction
Hemostasis and vasoconstriction play distinct clinical roles in controlling bleeding; hemostasis involves a complex cascade of platelet aggregation and coagulation factors to form a stable clot, essential in surgical and trauma settings to prevent excessive blood loss. Vasoconstriction, the narrowing of blood vessels mediated by smooth muscle contraction, serves as an immediate response to vascular injury, reducing blood flow but not forming a clot, crucial in initial hemorrhage control. Understanding their interplay guides effective management of bleeding disorders and the development of therapeutic agents targeting platelet function or vascular tone.
Disorders Related to Hemostasis and Vasoconstriction
Disorders related to hemostasis include hemophilia, characterized by impaired blood clotting due to factor VIII or IX deficiencies, and thrombocytopenia, marked by low platelet counts leading to excessive bleeding. Vasoconstriction disorders involve conditions such as Raynaud's phenomenon, where excessive narrowing of blood vessels causes restricted blood flow, and hypertension, often linked to chronic vasoconstriction increasing vascular resistance. Both hemostatic and vasoconstrictive dysfunctions can contribute to serious cardiovascular complications like stroke and myocardial infarction.
Summary: Integrating Hemostasis and Vasoconstriction for Vascular Health
Hemostasis and vasoconstriction are crucial physiological processes that work together to maintain vascular integrity and prevent excessive blood loss. Vasoconstriction rapidly reduces blood flow by narrowing blood vessels at injury sites, while hemostasis stabilizes clots through platelet aggregation and fibrin formation. Integrating these mechanisms ensures immediate vascular repair and long-term vessel stability critical for overall circulatory health.
Hemostasis Infographic
 libterm.com
libterm.com