Medicalization refers to the process by which non-medical issues become defined and treated as medical problems, often involving the use of medical language, diagnosis, and interventions. This shift can affect various aspects of life, from normal aging to behavioral traits, impacting how society perceives and manages these conditions. Explore the full article to understand the implications of medicalization on your health and well-being.
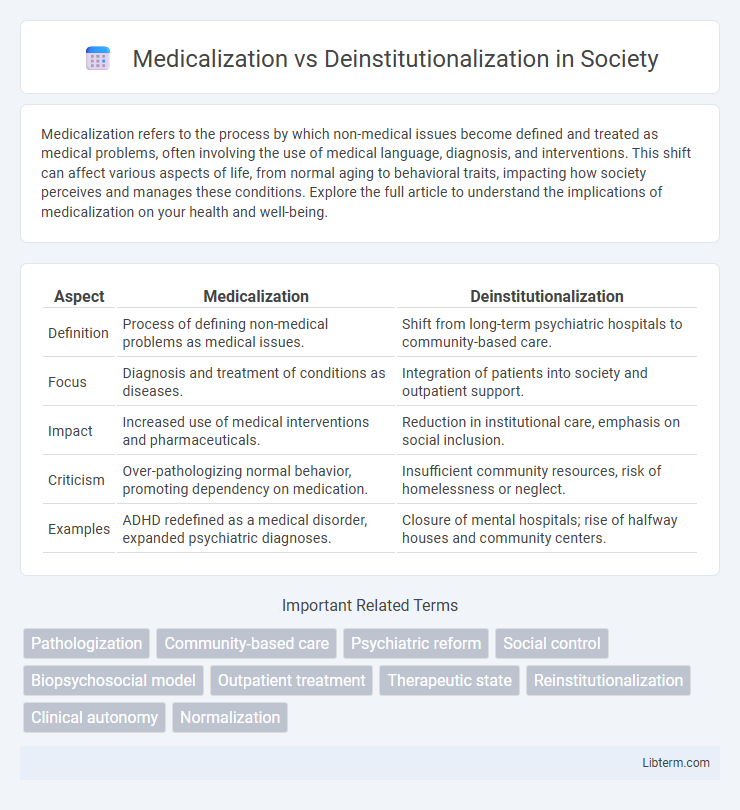
Table of Comparison
| Aspect | Medicalization | Deinstitutionalization |
|---|---|---|
| Definition | Process of defining non-medical problems as medical issues. | Shift from long-term psychiatric hospitals to community-based care. |
| Focus | Diagnosis and treatment of conditions as diseases. | Integration of patients into society and outpatient support. |
| Impact | Increased use of medical interventions and pharmaceuticals. | Reduction in institutional care, emphasis on social inclusion. |
| Criticism | Over-pathologizing normal behavior, promoting dependency on medication. | Insufficient community resources, risk of homelessness or neglect. |
| Examples | ADHD redefined as a medical disorder, expanded psychiatric diagnoses. | Closure of mental hospitals; rise of halfway houses and community centers. |
Understanding Medicalization: Definition and Scope
Medicalization refers to the process by which non-medical problems become defined and treated as medical issues, often involving diagnosis, treatment, and intervention by healthcare professionals. This concept encompasses a wide scope, including the expansion of medical authority into everyday life domains such as mental health, childbirth, and aging. Understanding medicalization requires examining how social, cultural, and economic factors influence the framing of behaviors and conditions within a medical context.
Deinstitutionalization Explained: A Paradigm Shift
Deinstitutionalization represents a paradigm shift in mental health care, moving away from long-term psychiatric hospital confinement toward community-based treatment and integration. This approach emphasizes patient autonomy, social inclusion, and access to outpatient services, reducing reliance on institutional settings. Key outcomes include improved quality of life and reduced stigma for individuals with mental illness through personalized support in everyday environments.
Historical Context: Evolution of Mental Health Care
The evolution of mental health care witnessed a shift from the medicalization approach, which emphasized psychiatric diagnosis and hospital-based treatment, to deinstitutionalization starting in the mid-20th century. This transition was driven by rising concerns over the conditions of psychiatric asylums, advances in psychotropic medications, and a growing movement toward community-based care. Historical policies such as the Community Mental Health Act of 1963 in the United States marked a pivotal moment, promoting outpatient services and reducing reliance on large institutions.
Key Differences: Medicalization vs Deinstitutionalization
Medicalization refers to the process by which non-medical issues become defined and treated as medical problems, often involving diagnosis, medication, and clinical intervention. Deinstitutionalization involves the systematic reduction of long-term psychiatric hospital care, emphasizing community-based treatment and integration of patients into society. Key differences include medicalization's focus on expanding medical authority and interventions, whereas deinstitutionalization prioritizes reducing institutional dependency and promoting social support structures.
Social Impacts of Medicalization
Medicalization shifts mental health issues from social contexts to medical diagnoses, often leading to increased dependency on pharmaceutical treatments and healthcare systems. This process can stigmatize individuals by framing behaviors as medical problems rather than social or environmental issues, impacting self-identity and societal attitudes. The social implications include reduced emphasis on community-based solutions and potential neglect of underlying social determinants of health.
Deinstitutionalization and Community-Based Care
Deinstitutionalization involves the systematic reduction of psychiatric hospital populations, promoting the shift toward community-based care that emphasizes treatment within the least restrictive environments. Community-based care integrates multidisciplinary approaches, including outpatient therapy, case management, and supported housing, to enhance patient autonomy and social inclusion. This model significantly reduces hospitalization rates and improves long-term outcomes for individuals with mental health disorders by fostering resilience and community support networks.
Benefits and Drawbacks of Each Approach
Medicalization emphasizes diagnosing and treating mental health disorders through clinical interventions, enabling access to advanced medications and therapies that can improve patient outcomes. Deinstitutionalization aims to reduce reliance on long-term psychiatric hospitalization, promoting community-based care and social integration but may lead to inadequate support and increased homelessness for some individuals. While medicalization risks over-pathologizing normal behaviors, deinstitutionalization can strain community resources, highlighting the need for balanced, patient-centered care models.
Policy Implications: Shaping Mental Health Systems
Medicalization expands psychiatric diagnoses, increasing reliance on pharmacological treatments and shaping policies that prioritize clinical interventions over social supports. Deinstitutionalization promotes community-based care models, driving legislative reforms to fund outpatient services and integrate mental health care into primary health systems. Policymakers balance these trends by creating frameworks that ensure access, emphasize recovery, and address systemic gaps in mental health resources.
Contemporary Debates and Criticisms
Contemporary debates on medicalization vs deinstitutionalization center on the balance between clinical treatment and social integration for mental health patients. Critics argue medicalization risks pathologizing normal behaviors and over-reliance on pharmaceuticals, while deinstitutionalization faces challenges like insufficient community resources and increased homelessness among the mentally ill. Evidence-based policies emphasize integrated care models addressing both medical needs and social determinants to improve patient outcomes.
Future Directions in Mental Health Treatment
Future directions in mental health treatment emphasize integrating advanced medicalization techniques with community-based deinstitutionalization efforts to enhance patient autonomy and personalized care. Innovations in neuropsychiatric pharmacology and digital therapeutics aim to reduce hospitalization rates while improving symptom management outside institutional settings. Emphasizing holistic, interdisciplinary approaches that combine medical, psychological, and social support systems will drive more sustainable and effective mental health outcomes.
Medicalization Infographic
 libterm.com
libterm.com