Subclinical hypothyroidism occurs when thyroid-stimulating hormone (TSH) levels are elevated, but free thyroid hormone levels remain within normal ranges, often presenting without obvious symptoms. Early detection and monitoring are important since untreated subclinical hypothyroidism can progress to overt hypothyroidism or impact cardiovascular health. Explore this article to understand how subclinical hypothyroidism affects your health and the best approaches to management.
Table of Comparison
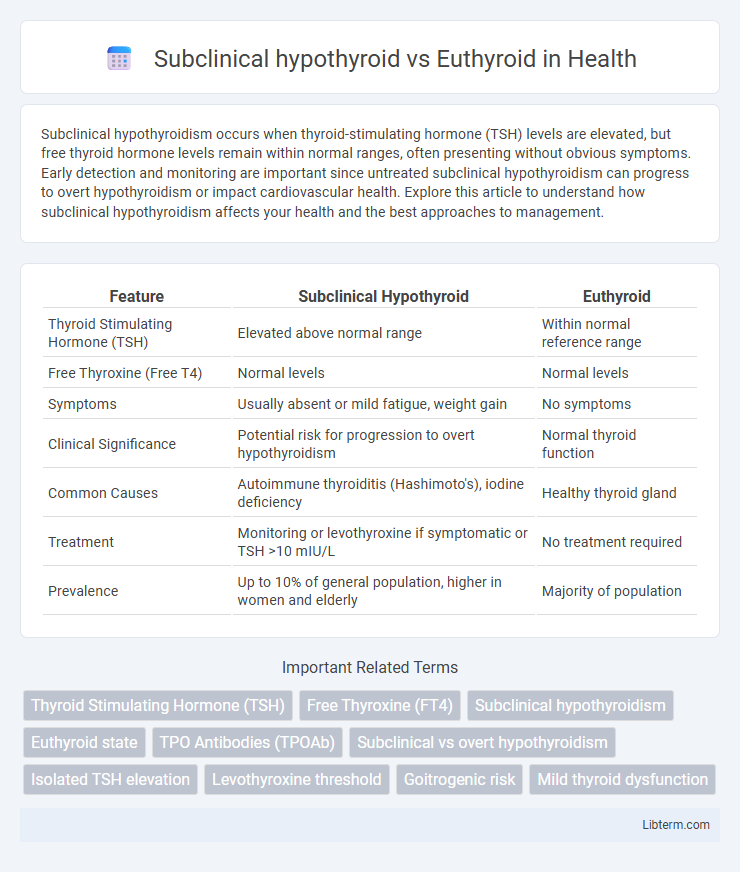
| Feature | Subclinical Hypothyroid | Euthyroid |
|---|---|---|
| Thyroid Stimulating Hormone (TSH) | Elevated above normal range | Within normal reference range |
| Free Thyroxine (Free T4) | Normal levels | Normal levels |
| Symptoms | Usually absent or mild fatigue, weight gain | No symptoms |
| Clinical Significance | Potential risk for progression to overt hypothyroidism | Normal thyroid function |
| Common Causes | Autoimmune thyroiditis (Hashimoto's), iodine deficiency | Healthy thyroid gland |
| Treatment | Monitoring or levothyroxine if symptomatic or TSH >10 mIU/L | No treatment required |
| Prevalence | Up to 10% of general population, higher in women and elderly | Majority of population |
Overview of Thyroid Function
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (FT4) concentrations, indicating early or mild thyroid dysfunction without overt symptoms. In contrast, euthyroid status reflects normal TSH and thyroid hormone levels, maintaining metabolic homeostasis and physiological functions. Thyroid function plays a critical role in regulating metabolism, energy production, and organ function, making the differentiation between subclinical hypothyroid and euthyroid states essential for clinical decision-making.
Defining Subclinical Hypothyroidism
Subclinical hypothyroidism is characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (FT4) concentrations, differentiating it from euthyroid status where both TSH and FT4 remain within reference ranges. This condition often presents without overt symptoms, making biochemical evaluation crucial for diagnosis. Early identification of subclinical hypothyroidism aids in monitoring potential progression to overt hypothyroidism and guides clinical decision-making.
Understanding Euthyroid State
The euthyroid state represents normal thyroid function characterized by balanced levels of thyroid hormones (T3 and T4) and thyroid-stimulating hormone (TSH) within reference ranges, ensuring optimal metabolic activity and physiological homeostasis. This contrasts with subclinical hypothyroidism, where TSH levels are elevated above the normal range while free T3 and T4 remain within normal limits, indicating early thyroid dysfunction without overt symptoms. Understanding the euthyroid state is critical for distinguishing normal thyroid hormone regulation from subtle endocrine imbalances that may precede clinical hypothyroidism.
Diagnostic Criteria: Subclinical vs Euthyroid
Subclinical hypothyroidism is characterized by elevated serum thyroid-stimulating hormone (TSH) levels, typically between 4.5 and 10 mIU/L, while free thyroxine (FT4) remains within the normal reference range. Euthyroid individuals exhibit TSH and FT4 levels within standard laboratory reference intervals, indicating normal thyroid function. Accurate diagnosis relies on sensitive TSH assays and repeat testing to distinguish transient TSH elevations from persistent subclinical hypothyroidism.
Common Causes and Risk Factors
Subclinical hypothyroidism is frequently caused by autoimmune thyroiditis, iodine deficiency, or certain medications such as lithium and amiodarone, while euthyroid individuals maintain normal thyroid hormone levels despite similar risk exposures. Risk factors for subclinical hypothyroidism include female gender, advanced age, family history of thyroid disease, and iodine insufficiency, whereas euthyroid status is typically observed in healthy individuals without these risk factors. Understanding these disparities in etiology and risk helps direct early diagnosis and management strategies in at-risk populations.
Clinical Signs and Symptoms Comparison
Subclinical hypothyroidism often presents with subtle or no overt clinical signs, but may include mild fatigue, weight gain, and cold intolerance, whereas euthyroid individuals display normal metabolic function without these symptoms. Laboratory tests reveal elevated thyroid-stimulating hormone (TSH) with normal free thyroxine (FT4) in subclinical hypothyroid patients, contrasting with normal TSH and FT4 levels in euthyroid individuals. Subclinical hypothyroidism may lead to cardiovascular changes such as diastolic hypertension not typically observed in euthyroid subjects.
Laboratory Findings and Interpretation
Subclinical hypothyroidism is characterized by elevated serum thyroid-stimulating hormone (TSH) levels with normal free thyroxine (FT4) and free triiodothyronine (FT3) concentrations, indicating early thyroid dysfunction without overt hormone deficiency. In contrast, euthyroid status presents with normal TSH, FT4, and FT3 values, reflecting typical thyroid gland function. Interpretation of laboratory findings requires assessing TSH as the primary sensitive marker, with elevated TSH and normal thyroid hormones suggesting subclinical hypothyroidism, while all parameters within reference ranges confirm euthyroid physiology.
Health Implications and Potential Complications
Subclinical hypothyroidism, characterized by elevated thyroid-stimulating hormone (TSH) levels with normal free thyroxine (T4), may increase risks of cardiovascular disease, lipid abnormalities, and progression to overt hypothyroidism compared to euthyroid individuals with balanced thyroid function. Research highlights subclinical hypothyroidism's association with endothelial dysfunction, increased carotid intima-media thickness, and subtle neurocognitive impairments, which are absent in euthyroid states. Early detection and monitoring are crucial to mitigate potential complications such as heart failure, infertility, and metabolic syndrome in patients with subclinical hypothyroidism.
Current Treatment Approaches
Subclinical hypothyroidism treatment primarily involves careful monitoring of thyroid-stimulating hormone (TSH) levels and selective levothyroxine therapy in patients with TSH above 10 mIU/L or those exhibiting symptoms. Euthyroid individuals do not require thyroid hormone supplementation but benefit from regular thyroid function assessments to detect any progression toward hypothyroidism. Current clinical guidelines recommend individualized treatment based on patient age, comorbidities, and risk factors to optimize outcomes and prevent overt thyroid dysfunction.
Prognosis and Long-Term Management
Subclinical hypothyroidism often presents with mildly elevated thyroid-stimulating hormone (TSH) levels and normal free thyroxine (T4), requiring careful monitoring due to variable progression risk to overt hypothyroidism. Euthyroid individuals maintain stable thyroid hormone levels and generally exhibit a favorable prognosis without the need for thyroid-specific treatment. Long-term management of subclinical hypothyroidism may involve periodic thyroid function tests and consideration of levothyroxine therapy in cases with symptoms, pregnancy, or significant TSH elevation above 10 mIU/L.
Subclinical hypothyroid Infographic
 libterm.com
libterm.com