Neutropenia and leukopenia refer to conditions characterized by abnormally low levels of neutrophils and white blood cells, respectively, which can compromise your immune system and increase infection risk. Understanding the causes, symptoms, and treatment options is essential for managing these blood disorders effectively. Explore the rest of the article to learn how to recognize and address neutropenia and leukopenia.
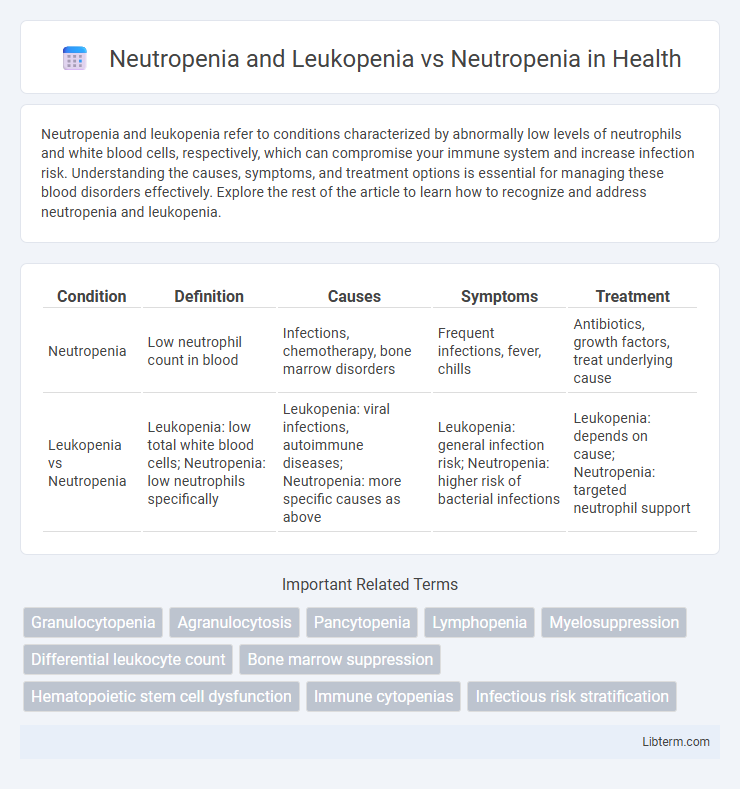
Table of Comparison
| Condition | Definition | Causes | Symptoms | Treatment |
|---|---|---|---|---|
| Neutropenia | Low neutrophil count in blood | Infections, chemotherapy, bone marrow disorders | Frequent infections, fever, chills | Antibiotics, growth factors, treat underlying cause |
| Leukopenia vs Neutropenia | Leukopenia: low total white blood cells; Neutropenia: low neutrophils specifically | Leukopenia: viral infections, autoimmune diseases; Neutropenia: more specific causes as above | Leukopenia: general infection risk; Neutropenia: higher risk of bacterial infections | Leukopenia: depends on cause; Neutropenia: targeted neutrophil support |
Introduction to Neutropenia and Leukopenia
Neutropenia and leukopenia both involve a decrease in white blood cells, but neutropenia specifically refers to a reduced number of neutrophils, a type of white blood cell crucial for fighting bacterial infections. Leukopenia is a broader term indicating a decrease in the total white blood cell count, which can include reductions in neutrophils, lymphocytes, or other white blood cells. Understanding the distinction between neutropenia and leukopenia is essential for diagnosing and managing underlying causes such as infections, bone marrow disorders, or the effects of chemotherapy.
Defining Neutropenia: Causes and Diagnosis
Neutropenia is characterized by an abnormally low count of neutrophils, a type of white blood cell essential for fighting infections. Causes include bone marrow disorders, autoimmune diseases, chemotherapy, and severe infections, which impair neutrophil production or increase destruction. Diagnosis typically involves complete blood count (CBC) tests, bone marrow biopsy, and evaluation of underlying conditions to distinguish neutropenia from leukopenia, which involves a broader reduction in white blood cells.
Understanding Leukopenia: Broader Implications
Leukopenia encompasses a reduction in the total white blood cell count, including neutrophils, lymphocytes, and monocytes, making it a broader condition than neutropenia, which specifically refers to a decrease in neutrophils. Understanding leukopenia is crucial because it reflects a generalized vulnerability to infections, affecting various immune responses beyond neutrophil-mediated defenses. Clinical management requires addressing the underlying causes and monitoring multiple immune parameters to prevent severe infections and guide targeted treatments.
Neutropenia vs Leukopenia: Key Differences
Neutropenia specifically refers to an abnormally low count of neutrophils, a type of white blood cell essential for fighting bacterial infections, while leukopenia denotes a reduced overall white blood cell count, including neutrophils, lymphocytes, and other immune cells. Neutropenia increases susceptibility primarily to bacterial and fungal infections, whereas leukopenia signals a broader immune deficiency that compromises the body's ability to combat various pathogens. Laboratory tests measuring absolute neutrophil count (ANC) and total white blood cell (WBC) count are critical for differentiating neutropenia from leukopenia and guiding targeted clinical management.
Common Causes of Neutropenia and Leukopenia
Common causes of neutropenia and leukopenia include bone marrow disorders such as aplastic anemia and myelodysplastic syndromes, infections like viral hepatitis and HIV, and autoimmune diseases including systemic lupus erythematosus. Chemotherapy, radiation therapy, and certain medications can suppress bone marrow function, leading to decreased neutrophil and white blood cell counts. Nutritional deficiencies, particularly vitamin B12 and folate, can also contribute to the development of neutropenia and leukopenia.
Clinical Symptoms and Presentation
Neutropenia primarily presents with recurrent bacterial and fungal infections, fever, and mucosal ulcerations due to the decreased number of neutrophils compromising the innate immune response. Leukopenia encompasses a broader reduction in white blood cells, causing increased susceptibility to a wider range of infections including viral and bacterial, along with symptoms such as fatigue, fever, and sore throat. Clinical differentiation is based on specific white blood cell counts and associated infections, with neutropenia showing isolated neutrophil decline and leukopenia reflecting multiple white cell line decreases.
Diagnostic Strategies for Neutropenia and Leukopenia
Diagnostic strategies for neutropenia and leukopenia emphasize comprehensive blood count analysis to quantify absolute neutrophil and white blood cell levels, distinguishing neutropenia from broader leukopenia. Bone marrow biopsy and flow cytometry provide critical insights into hematopoietic function and potential underlying marrow pathologies. Molecular and genetic testing aids in identifying congenital or acquired etiologies, informing targeted treatment plans for neutropenic and leukopenic patients.
Treatment Approaches: Neutropenia vs Leukopenia
Treatment approaches for neutropenia primarily focus on boosting neutrophil counts using granulocyte colony-stimulating factors (G-CSF) such as filgrastim and managing underlying causes like infections or chemotherapy-induced myelosuppression. Leukopenia treatment is broader, addressing overall white blood cell deficiency by targeting specific etiologies including bone marrow disorders, autoimmune diseases, or medication-induced suppression, with interventions ranging from immunosuppressants to hematopoietic growth factors. Both conditions require close monitoring for infection risk, but neutropenia management is often more aggressive due to the critical role of neutrophils in bacterial defense.
Prognosis and Complications
Neutropenia, characterized by a significant reduction in neutrophil count, primarily increases the risk of severe bacterial and fungal infections, leading to potential complications such as sepsis and delayed wound healing. Leukopenia encompasses a broader reduction in white blood cells, including neutrophils, lymphocytes, and monocytes, often resulting in a more complex immune deficiency with higher susceptibility to viral, bacterial, and fungal infections. Prognosis in neutropenia is generally better when isolated and promptly managed, while leukopenia may indicate underlying bone marrow failure or systemic diseases, often carrying a worse prognosis due to multifaceted immune compromise.
Prevention and Patient Management Strategies
Effective prevention and patient management strategies for neutropenia and leukopenia include regular monitoring of white blood cell counts and avoiding exposure to infections through hygiene and protective measures. Use of growth factors like granulocyte colony-stimulating factor (G-CSF) can stimulate neutrophil production, reducing the risk of severe infections in both conditions. Patient education on early infection signs and prompt medical intervention is critical to minimize complications and improve outcomes.
Neutropenia and Leukopenia Infographic
 libterm.com
libterm.com