Necrotic tissue results from the death of cells due to injury, infection, or inadequate blood supply, leading to irreversible damage and potential complications if untreated. Early identification and proper medical intervention are crucial to prevent the spread of necrosis and promote healing. Discover more about the causes, symptoms, and treatment options for necrotic conditions in the rest of this article.
Table of Comparison
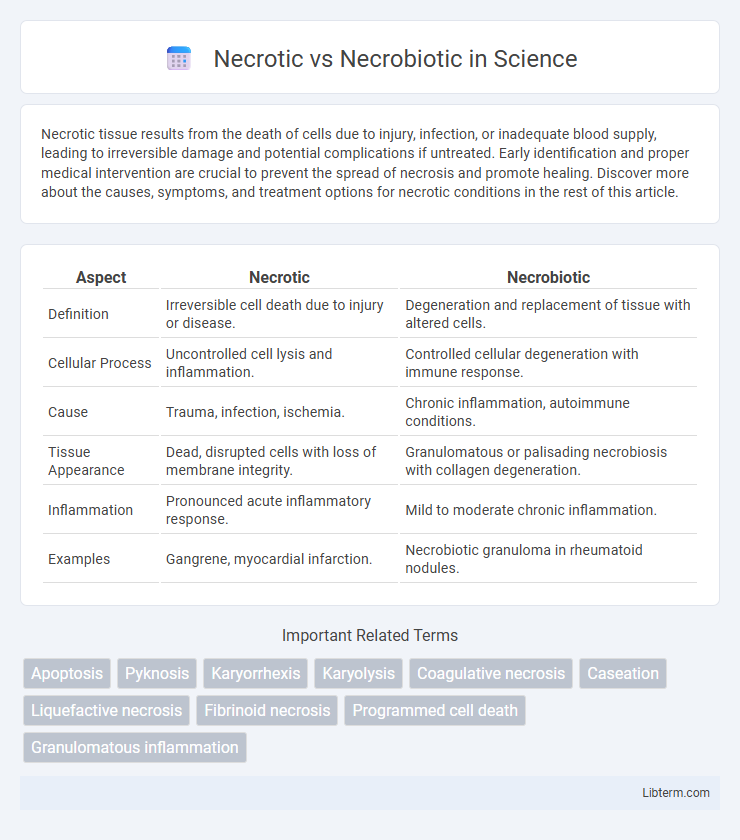
| Aspect | Necrotic | Necrobiotic |
|---|---|---|
| Definition | Irreversible cell death due to injury or disease. | Degeneration and replacement of tissue with altered cells. |
| Cellular Process | Uncontrolled cell lysis and inflammation. | Controlled cellular degeneration with immune response. |
| Cause | Trauma, infection, ischemia. | Chronic inflammation, autoimmune conditions. |
| Tissue Appearance | Dead, disrupted cells with loss of membrane integrity. | Granulomatous or palisading necrobiosis with collagen degeneration. |
| Inflammation | Pronounced acute inflammatory response. | Mild to moderate chronic inflammation. |
| Examples | Gangrene, myocardial infarction. | Necrobiotic granuloma in rheumatoid nodules. |
Introduction to Necrosis and Necrobiosis
Necrosis describes the uncontrolled, pathological death of cells due to injury, infection, or lack of blood supply, resulting in cellular swelling, membrane rupture, and inflammation. Necrobiosis refers to the physiologic, regulated process of cell aging and natural cell death without eliciting an inflammatory response, often observed in connective tissues and granulomas. Understanding necrosis and necrobiosis is crucial for distinguishing between disease-related tissue damage and normal cellular turnover in histopathology.
Definition of Necrotic Changes
Necrotic changes refer to the irreversible death of cells or tissues caused by factors such as infection, toxins, or ischemia, resulting in the loss of cell membrane integrity and enzymatic digestion of cellular components. In necrosis, the affected tissue often shows coagulative or liquefactive patterns, leading to inflammation in surrounding areas. Necrotic changes differ from necrobiotic alterations, which involve a more controlled, degenerative cell process typically seen in chronic inflammatory conditions.
Definition of Necrobiotic Changes
Necrobiotic changes refer to the process of controlled cell death involving the degradation of cellular components while maintaining tissue framework, often seen in chronic inflammatory conditions like necrobiosis lipoidica. Unlike necrotic changes, which result in uncontrolled cell destruction and tissue disintegration, necrobiotic alterations preserve the overall architecture despite cellular damage. This distinction is critical in histopathology for accurate diagnosis and treatment planning.
Pathophysiology: Necrotic vs Necrobiotic Processes
Necrotic processes involve irreversible cell injury leading to cell death, characterized by cellular swelling, membrane rupture, and inflammation due to the release of intracellular contents. Necrobiotic processes, often observed in chronic inflammatory conditions, feature granulomatous inflammation with collagen degeneration and macrophage infiltration surrounding altered tissue. The distinction lies in necrosis representing acute cell death, whereas necrobiosis describes a more controlled, chronic tissue degradation linked to immune-mediated mechanisms.
Histological Features: Key Differences
Necrotic tissue displays extensive coagulative necrosis characterized by loss of nuclei, eosinophilic cytoplasm, and tissue architecture disruption on histological examination. Necrobiotic lesions typically exhibit palisading granulomas with central zones of collagen degeneration and mixed inflammatory infiltrate, often found in conditions like necrobiosis lipoidica. The key histological difference lies in the pattern of tissue damage: necrosis involves indiscriminate cell death, while necrobiosis shows organized, granulomatous inflammation with collagen degeneration.
Clinical Manifestations and Relevance
Necrotic tissue presents with features such as blackened, non-viable skin, severe pain, and potential systemic toxicity, indicating acute and often irreversible damage requiring urgent debridement. Necrobiotic changes typically manifest as localized, granulomatous plaques or nodules with central necrosis, commonly seen in conditions like necrobiosis lipoidica, reflecting a chronic inflammatory process with variable prognosis. Understanding these clinical manifestations aids in differentiating acute tissue death from chronic inflammatory necrosis, guiding appropriate therapeutic interventions and prognosis assessment.
Common Diseases Involving Necrosis
Common diseases involving necrosis include myocardial infarction, where cardiac tissue death occurs due to ischemia, and gangrene, characterized by widespread tissue necrosis often caused by infection or vascular occlusion. In contrast, necrobiotic granulomas, seen in conditions like rheumatoid arthritis and necrobiosis lipoidica, involve chronic inflammation with collagen degeneration rather than outright tissue death. Understanding these distinctions aids in accurate diagnosis and targeted treatment strategies for necrotic and necrobiotic pathologies.
Common Conditions Featuring Necrobiosis
Common conditions featuring necrobiosis include necrobiosis lipoidica, granuloma annulare, and rheumatoid nodules, all characterized by collagen degeneration with palisading histiocytes. In necrobiosis lipoidica, patients present with yellow-brown atrophic plaques primarily on the shins, often linked to diabetes mellitus. Granuloma annulare displays annular plaques with central clearing, while rheumatoid nodules are firm subcutaneous lumps associated with rheumatoid arthritis, both exhibiting necrobiotic changes on histology.
Diagnostic Approaches: Necrosis vs Necrobiosis
Diagnostic approaches for necrosis primarily rely on imaging techniques such as MRI and CT scans to identify tissue death characterized by cellular rupture and inflammation. In contrast, necrobiosis diagnosis involves histopathological examination revealing granulomatous inflammation and degenerative changes within collagen bundles. Biomarkers like elevated lactate dehydrogenase (LDH) levels support necrosis identification, while immunohistochemistry highlights inflammatory cells in necrobiosis cases.
Therapeutic Implications and Prognosis
Necrotic tissue typically indicates irreversible cell death with poor regenerative potential, necessitating aggressive debridement and often leading to complications like infection or chronic wounds, whereas necrobiotic lesions, characterized by a controlled chronic inflammatory process, may respond better to immunomodulatory therapies such as corticosteroids or biologics. Prognosis for necrotic conditions often depends on the extent of tissue damage and promptness of intervention, while necrobiotic disorders generally have a more favorable outcome if underlying inflammatory triggers are managed effectively. Understanding the distinct pathophysiology of necrotic versus necrobiotic processes is crucial for tailoring targeted treatments and improving patient outcomes.
Necrotic Infographic
 libterm.com
libterm.com