Bronchodilation refers to the widening of the airways in the lungs, which helps improve airflow and makes breathing easier, especially for individuals with respiratory conditions like asthma or COPD. This physiological process is often stimulated by medications such as beta-agonists or anticholinergics that relax the smooth muscles around the bronchi. Discover how bronchodilation affects your respiratory health and the treatments available by reading the rest of the article.
Table of Comparison
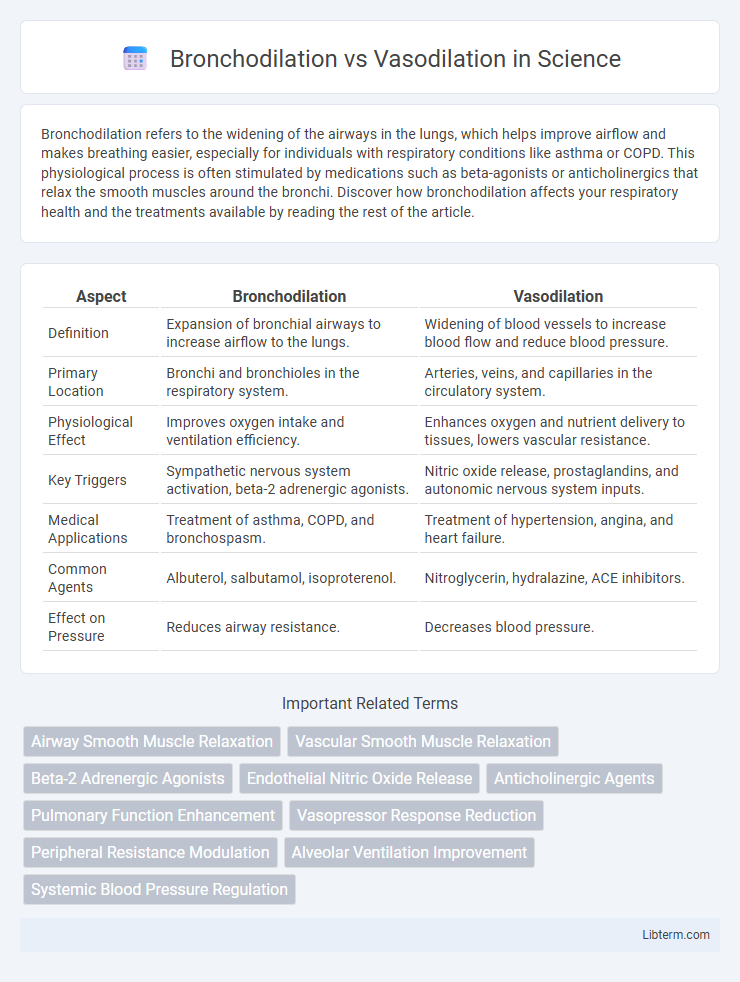
| Aspect | Bronchodilation | Vasodilation |
|---|---|---|
| Definition | Expansion of bronchial airways to increase airflow to the lungs. | Widening of blood vessels to increase blood flow and reduce blood pressure. |
| Primary Location | Bronchi and bronchioles in the respiratory system. | Arteries, veins, and capillaries in the circulatory system. |
| Physiological Effect | Improves oxygen intake and ventilation efficiency. | Enhances oxygen and nutrient delivery to tissues, lowers vascular resistance. |
| Key Triggers | Sympathetic nervous system activation, beta-2 adrenergic agonists. | Nitric oxide release, prostaglandins, and autonomic nervous system inputs. |
| Medical Applications | Treatment of asthma, COPD, and bronchospasm. | Treatment of hypertension, angina, and heart failure. |
| Common Agents | Albuterol, salbutamol, isoproterenol. | Nitroglycerin, hydralazine, ACE inhibitors. |
| Effect on Pressure | Reduces airway resistance. | Decreases blood pressure. |
Understanding Bronchodilation: Definition and Mechanisms
Bronchodilation refers to the widening of the bronchial airways resulting from the relaxation of smooth muscle in the respiratory tract, primarily driven by the activation of beta-2 adrenergic receptors. This physiological process increases airflow to the lungs, improving oxygen exchange and alleviating conditions like asthma and chronic obstructive pulmonary disease (COPD). Key mechanisms involve the release of cyclic AMP (cAMP) within smooth muscle cells, which inhibits muscle contraction and promotes airway relaxation.
What is Vasodilation? An Overview
Vasodilation refers to the widening of blood vessels resulting from the relaxation of the vascular smooth muscle, which leads to increased blood flow and decreased blood pressure. It plays a critical role in regulating body temperature, enhancing oxygen delivery to tissues, and facilitating the removal of metabolic waste. Key mediators of vasodilation include nitric oxide, prostacyclin, and endothelium-derived hyperpolarizing factors.
Key Physiological Processes: Bronchodilation vs Vasodilation
Bronchodilation involves the relaxation of smooth muscle in the bronchi and bronchioles, leading to an increase in airway diameter and improved airflow to the lungs. Vasodilation refers to the widening of blood vessels caused by the relaxation of vascular smooth muscle, which decreases vascular resistance and enhances blood flow. Both processes are regulated by signaling molecules such as nitric oxide and involve autonomic nervous system control, but target distinct tissue types with different physiological outcomes.
Primary Causes and Triggers
Bronchodilation primarily occurs due to the activation of beta-2 adrenergic receptors by catecholamines like epinephrine, which relaxes smooth muscles in the airways, commonly triggered by asthma medications or physical activity. Vasodilation results from the release of nitric oxide, prostacyclin, or histamine, leading to the relaxation of vascular smooth muscles, and is often induced by inflammatory responses, heat exposure, or certain medications such as calcium channel blockers. Both processes involve smooth muscle relaxation but are regulated by distinct signaling pathways and stimuli based on their functional roles in the respiratory and cardiovascular systems.
Main Functions in the Respiratory and Circulatory Systems
Bronchodilation primarily functions to widen the airways in the respiratory system, enhancing airflow and oxygen delivery to the lungs by relaxing the smooth muscles surrounding the bronchi and bronchioles. Vasodilation, occurring in the circulatory system, involves the expansion of blood vessels, particularly the arterioles, which increases blood flow, reduces vascular resistance, and facilitates efficient oxygen and nutrient transport to tissues. Both processes are vital for maintaining optimal respiratory gas exchange and circulatory dynamics, supporting overall cardiovascular and pulmonary health.
Medications Promoting Bronchodilation and Vasodilation
Medications promoting bronchodilation primarily include beta-2 agonists like albuterol and anticholinergics such as ipratropium, targeting airway smooth muscle relaxation to improve airflow in conditions like asthma and COPD. Vasodilation is commonly induced by drugs such as nitrates, calcium channel blockers, and ACE inhibitors, which act on vascular smooth muscle to reduce blood pressure and enhance blood flow in cardiovascular diseases. Understanding the distinct pharmacologic mechanisms of bronchodilators versus vasodilators enables targeted therapy for respiratory versus cardiovascular pathologies.
Clinical Applications: When and Why They're Used
Bronchodilation is primarily used in treating respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD) to relieve airway constriction and improve airflow. Vasodilation is employed in managing cardiovascular diseases like hypertension and angina by relaxing blood vessels to reduce blood pressure and enhance blood flow. Understanding the distinct mechanisms and target tissues is crucial for selecting appropriate therapies to optimize patient outcomes.
Side Effects and Contraindications
Bronchodilation primarily affects the respiratory system by relaxing airway smooth muscles, with side effects such as tachycardia, tremors, and nervousness, and is contraindicated in patients with cardiac arrhythmias or hypersensitivity to beta-agonists. Vasodilation targets blood vessels to lower blood pressure, potentially causing hypotension, dizziness, and reflex tachycardia, with contraindications including severe hypotension, aortic stenosis, and certain types of heart failure. Both processes require careful monitoring to avoid exacerbating underlying cardiovascular conditions or provoking adverse reactions.
Medical Conditions Linked to Bronchodilation and Vasodilation
Bronchodilation is primarily associated with respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD), where the relaxation of bronchial muscles improves airflow and alleviates symptoms like wheezing and shortness of breath. Vasodilation is linked to cardiovascular conditions including hypertension and peripheral artery disease, as the widening of blood vessels reduces blood pressure and enhances circulation. Medications targeting bronchodilation, like beta-2 agonists, and vasodilation, such as nitric oxide donors or calcium channel blockers, are critical in managing these diseases effectively.
Comparing Therapeutic Benefits and Risks
Bronchodilation primarily targets the respiratory system by relaxing bronchial muscles to improve airflow in conditions like asthma and COPD, while vasodilation affects blood vessels to lower blood pressure and enhance circulation, benefiting cardiovascular disorders. Therapeutic benefits of bronchodilators include rapid relief from bronchospasm and improved oxygen intake, whereas vasodilators reduce cardiac workload and prevent hypertension-related complications. Risks associated with bronchodilators involve tachycardia and palpitations, while vasodilators may cause hypotension, dizziness, and reflex tachycardia.
Bronchodilation Infographic
 libterm.com
libterm.com