Hyperemia refers to the increased blood flow to different tissues in the body, often resulting in redness and warmth in the affected area. This physiological response can be caused by inflammation, injury, or increased metabolic activity, and plays a critical role in healing and immune function. Explore this article to understand the causes, types, and clinical implications of hyperemia and how it may affect your health.
Table of Comparison
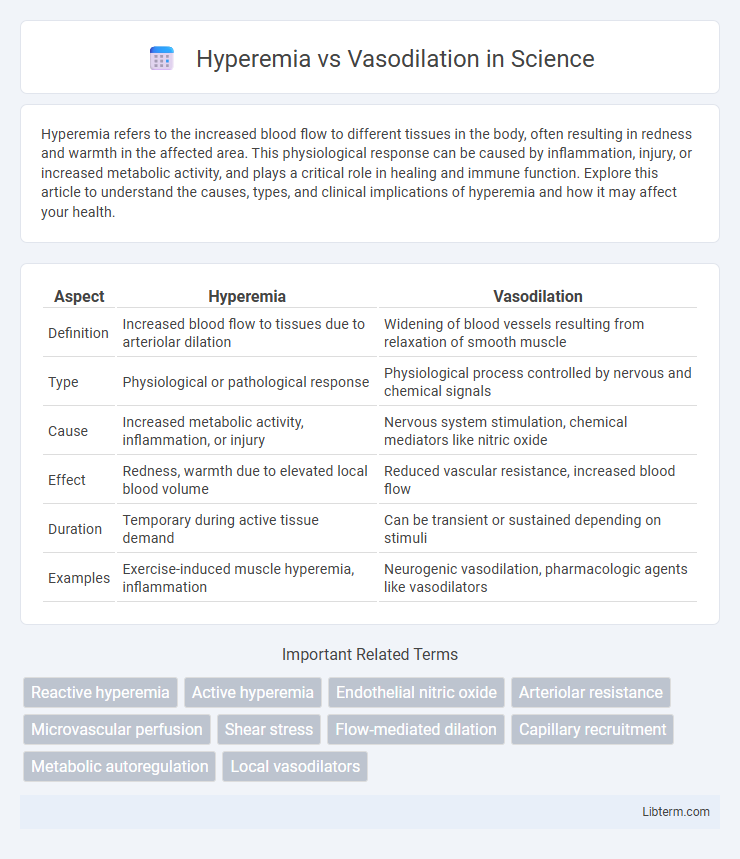
| Aspect | Hyperemia | Vasodilation |
|---|---|---|
| Definition | Increased blood flow to tissues due to arteriolar dilation | Widening of blood vessels resulting from relaxation of smooth muscle |
| Type | Physiological or pathological response | Physiological process controlled by nervous and chemical signals |
| Cause | Increased metabolic activity, inflammation, or injury | Nervous system stimulation, chemical mediators like nitric oxide |
| Effect | Redness, warmth due to elevated local blood volume | Reduced vascular resistance, increased blood flow |
| Duration | Temporary during active tissue demand | Can be transient or sustained depending on stimuli |
| Examples | Exercise-induced muscle hyperemia, inflammation | Neurogenic vasodilation, pharmacologic agents like vasodilators |
Introduction to Hyperemia and Vasodilation
Hyperemia refers to the increased blood flow to different tissues in the body, often due to metabolic activity or inflammation, resulting in redness and warmth. Vasodilation is the physiological process involving the relaxation of blood vessel walls, which leads to an increase in vessel diameter and enhances blood flow. Understanding the mechanisms of hyperemia and vasodilation is crucial for comprehending cardiovascular responses and tissue perfusion under various physiological and pathological conditions.
Defining Hyperemia: Causes and Types
Hyperemia refers to the increased blood flow to different tissues in the body, primarily caused by the dilation of arterioles and opening of capillary beds. It is classified into two main types: active hyperemia, which occurs due to increased metabolic activity such as muscle exercise or inflammation, and passive (or venous) hyperemia, which results from impaired venous drainage leading to blood accumulation. Common causes include physical activity, inflammation, and venous obstruction, all contributing to the distinct mechanisms underlying hyperemia versus simple vasodilation.
Understanding Vasodilation: Mechanisms and Triggers
Vasodilation is the physiological process where blood vessels widen due to relaxation of smooth muscle cells in the vessel walls, primarily influenced by factors such as nitric oxide, prostacyclin, and endothelium-derived hyperpolarizing factors. This expansion increases blood flow and decreases vascular resistance, playing a critical role in regulating blood pressure, temperature, and tissue perfusion. Understanding vasodilation involves exploring mechanisms triggered by chemical signals, shear stress, hypoxia, and neural stimulation that collectively modulate vascular tone for homeostasis and response to physiological demands.
Key Differences Between Hyperemia and Vasodilation
Hyperemia refers to the increased blood flow to specific tissues, usually due to metabolic demand or inflammation, whereas vasodilation is the widening of blood vessels caused by relaxation of vascular smooth muscle. Hyperemia results in redness and warmth as a consequence of elevated blood volume, while vasodilation primarily functions to regulate blood pressure and flow. Key differences include hyperemia being a localized process linked to tissue activity or injury, whereas vasodilation is a physiological mechanism that can occur systemically or locally to control vascular resistance.
Physiological Roles of Hyperemia
Hyperemia refers to the increased blood flow to a tissue or organ, primarily serving to enhance oxygen delivery and remove metabolic waste during heightened metabolic activity or injury. It is a crucial physiological response in processes such as exercise, inflammation, and tissue repair, facilitating nutrient and immune cell transport to affected areas. Unlike vasodilation, which is simply the widening of blood vessels, hyperemia encompasses the overall increase in blood volume within the microcirculation, reflecting active or reactive adjustment in tissue perfusion.
Vasodilation in Cardiovascular Regulation
Vasodilation plays a critical role in cardiovascular regulation by relaxing smooth muscle cells within blood vessel walls, thereby increasing vessel diameter and enhancing blood flow to tissues. This process reduces systemic vascular resistance and helps to lower blood pressure, ensuring adequate oxygen delivery during increased metabolic demands. Unlike hyperemia, which refers to increased blood flow due to elevated perfusion, vasodilation actively modulates vascular tone through endothelial factors such as nitric oxide and prostacyclin.
Clinical Significance: Hyperemia vs Vasodilation
Hyperemia is a physiologic increase in blood flow to tissues often indicative of inflammation or active metabolic demand, crucial for wound healing and tissue repair, whereas vasodilation refers to the widening of blood vessels that can be pharmacologically induced to manage hypertension or improve tissue perfusion. Clinically, hyperemia is used as a diagnostic sign in conditions such as infection or trauma, while vasodilation is a targeted therapeutic mechanism in cardiovascular diseases and shock management. Understanding the distinctions aids in tailoring interventions for circulatory disorders and optimizing tissue oxygenation.
Diagnostic Methods for Hyperemia and Vasodilation
Diagnostic methods for hyperemia primarily include clinical examination and imaging techniques such as Doppler ultrasound, which evaluates increased blood flow in affected tissues. For vasodilation, measurement often involves assessing vascular diameter changes via techniques like laser Doppler flowmetry and plethysmography to quantify blood vessel expansion. Advanced imaging modalities like functional MRI can also differentiate hyperemia from vasodilation by analyzing tissue perfusion and vascular reactivity.
Therapeutic Approaches Targeting Hyperemia and Vasodilation
Therapeutic approaches targeting hyperemia and vasodilation primarily focus on modulating blood flow to reduce inflammation and enhance tissue perfusion. Pharmacological agents such as vasodilators, including nitric oxide donors and calcium channel blockers, are used to induce controlled vasodilation in ischemic tissues, while anti-inflammatory drugs help manage hyperemia by reducing excessive blood flow and edema. Emerging therapies involve targeting endothelial function and microvascular regulation to optimize treatment outcomes in conditions like peripheral artery disease and inflammatory disorders.
Conclusion: Comparing Hyperemia and Vasodilation in Health and Disease
Hyperemia and vasodilation both involve increased blood flow but differ in mechanisms and clinical significance. Hyperemia refers to active arterial dilation associated with increased metabolic demand or inflammation, whereas vasodilation encompasses passive relaxation of blood vessel walls often induced by pharmacological agents or neural signals. Understanding these distinctions aids in diagnosing vascular conditions and tailoring treatments for cardiovascular, inflammatory, and ischemic diseases.
Hyperemia Infographic
 libterm.com
libterm.com