Vasoconstriction is the narrowing of blood vessels caused by the contraction of muscular walls, which increases blood pressure and reduces blood flow to certain areas. This physiological process is essential for regulating body temperature and directing blood to vital organs during stress or injury. Discover how vasoconstriction affects your health and the mechanisms behind it in the rest of this article.
Table of Comparison
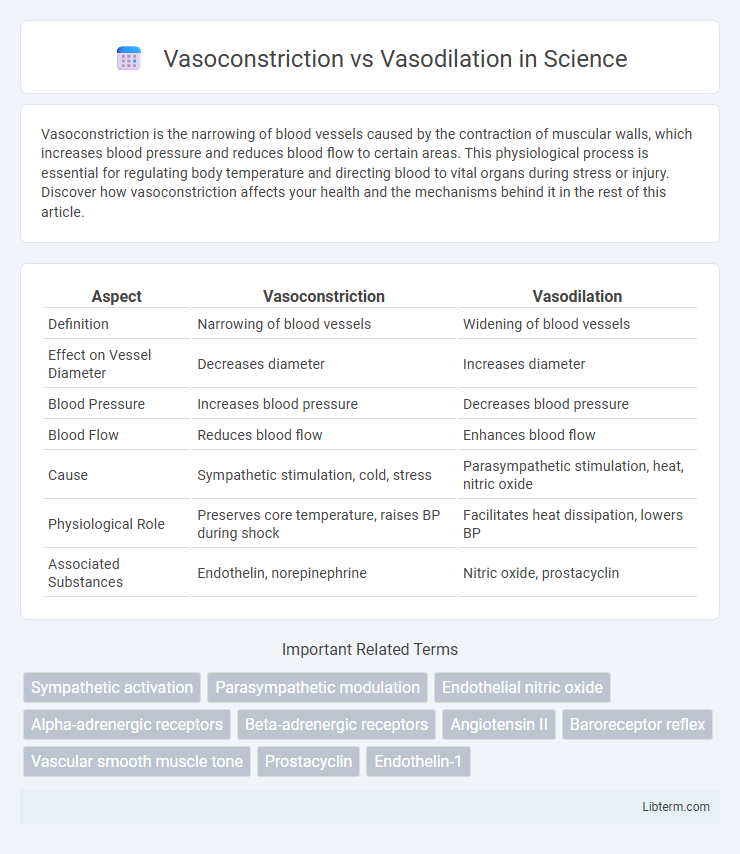
| Aspect | Vasoconstriction | Vasodilation |
|---|---|---|
| Definition | Narrowing of blood vessels | Widening of blood vessels |
| Effect on Vessel Diameter | Decreases diameter | Increases diameter |
| Blood Pressure | Increases blood pressure | Decreases blood pressure |
| Blood Flow | Reduces blood flow | Enhances blood flow |
| Cause | Sympathetic stimulation, cold, stress | Parasympathetic stimulation, heat, nitric oxide |
| Physiological Role | Preserves core temperature, raises BP during shock | Facilitates heat dissipation, lowers BP |
| Associated Substances | Endothelin, norepinephrine | Nitric oxide, prostacyclin |
Introduction to Vasoconstriction and Vasodilation
Vasoconstriction refers to the narrowing of blood vessels resulting from the contraction of vascular smooth muscle, which decreases blood flow and raises blood pressure. Vasodilation is the widening of blood vessels caused by relaxation of the smooth muscle cells, leading to increased blood flow and reduced blood pressure. These mechanisms regulate systemic vascular resistance and play critical roles in maintaining homeostasis and controlling tissue perfusion.
Definition of Vasoconstriction
Vasoconstriction refers to the narrowing of blood vessels resulting from the contraction of the muscular wall of the vessels, particularly the large arteries and small arterioles. This physiological process reduces blood flow and increases blood pressure by decreasing the vessel diameter. Vasodilation, in contrast, involves the relaxation of these muscular walls, leading to the widening of blood vessels and enhanced blood flow.
Definition of Vasodilation
Vasodilation is the physiological process involving the widening of blood vessels, primarily due to the relaxation of smooth muscle cells in the vessel walls. This expansion decreases vascular resistance and increases blood flow, enhancing oxygen and nutrient delivery to tissues. Vasodilation contrasts with vasoconstriction, where blood vessels narrow, increasing resistance and reducing blood flow.
Mechanisms Underlying Vasoconstriction
Vasoconstriction involves the narrowing of blood vessels triggered by the contraction of vascular smooth muscle cells, primarily regulated by the sympathetic nervous system through norepinephrine release acting on alpha-1 adrenergic receptors. Calcium ion influx and activation of the RhoA/Rho kinase pathway enhance smooth muscle contraction, reducing vessel diameter and increasing vascular resistance. Endothelin-1 and angiotensin II are potent vasoconstrictors that amplify this process by promoting calcium release and sensitizing contractile proteins within the vascular smooth muscle.
Mechanisms Underlying Vasodilation
Vasodilation occurs through the relaxation of vascular smooth muscle cells, primarily mediated by the release of nitric oxide (NO) from endothelial cells, which activates guanylate cyclase and increases cyclic GMP levels, leading to smooth muscle relaxation. Other key mediators include prostacyclin and endothelium-derived hyperpolarizing factors (EDHFs) that contribute to vasodilation by promoting potassium channel opening and hyperpolarization of smooth muscle cells. The inhibition of calcium influx in vascular smooth muscle cells also plays a critical role in reducing contraction and enhancing vessel diameter during vasodilation.
Key Differences: Vasoconstriction vs Vasodilation
Vasoconstriction involves the narrowing of blood vessels due to the contraction of muscular walls, leading to increased blood pressure and reduced blood flow, whereas vasodilation entails the widening of blood vessels through muscle relaxation, resulting in decreased blood pressure and enhanced blood flow. Key physiological effects of vasoconstriction include heat conservation and redirecting blood to vital organs, while vasodilation primarily facilitates heat dissipation and increased oxygen delivery to tissues. These opposing mechanisms regulate vascular resistance and play crucial roles in maintaining homeostasis during stress, temperature changes, and metabolic demand.
Physiological Roles in the Human Body
Vasoconstriction reduces blood vessel diameter, increasing vascular resistance and blood pressure to regulate temperature and maintain blood flow to vital organs during stress. Vasodilation expands blood vessels, decreasing resistance and enhancing blood flow to tissues, facilitating oxygen delivery and waste removal during exercise or heat exposure. These mechanisms are critical for homeostasis, controlling perfusion, and adapting to physiological demands such as injury response and thermoregulation.
Factors Influencing Vasoconstriction and Vasodilation
Factors influencing vasoconstriction include cold temperatures, sympathetic nervous system activation releasing norepinephrine, and elevated levels of vasoconstrictor substances such as endothelin and angiotensin II. Vasodilation is primarily promoted by increased nitric oxide production, the presence of vasodilatory substances like prostacyclin and bradykinin, as well as elevated carbon dioxide levels and decreased oxygen concentration in tissues. Hormonal influences, local metabolic factors, and neural inputs collectively regulate the balance between vasoconstriction and vasodilation, impacting blood flow and tissue oxygenation.
Health Implications and Disorders
Vasoconstriction, the narrowing of blood vessels, reduces blood flow and increases blood pressure, contributing to conditions like hypertension and peripheral artery disease. In contrast, vasodilation, the widening of blood vessels, enhances blood flow and lowers blood pressure but can lead to hypotension and shock if excessive. Imbalances in these vascular processes are critical in managing cardiovascular health, affecting risks of heart attacks, strokes, and chronic vascular disorders.
Therapeutic Approaches and Clinical Applications
Vasoconstriction and vasodilation play crucial roles in managing blood flow and pressure, with therapeutic approaches targeting specific receptors to treat cardiovascular conditions. Vasoconstrictors such as alpha-agonists are used clinically to increase blood pressure in hypotensive states and improve perfusion in shock, whereas vasodilators including nitrates, calcium channel blockers, and ACE inhibitors reduce vascular resistance to manage hypertension, angina, and heart failure. Advanced clinical applications involve personalized modulation of vascular tone, leveraging pharmacogenomics to optimize drug efficacy and minimize adverse effects in disorders like peripheral artery disease and pulmonary hypertension.
Vasoconstriction Infographic
 libterm.com
libterm.com