Asylum-based care provides essential support and protection for individuals seeking refuge from persecution, ensuring access to medical, psychological, and social services within a safe environment. This approach focuses on addressing the unique needs of asylum seekers while fostering integration and resilience. Discover how asylum-based care can impact your understanding of human rights and social justice in the full article.
Table of Comparison
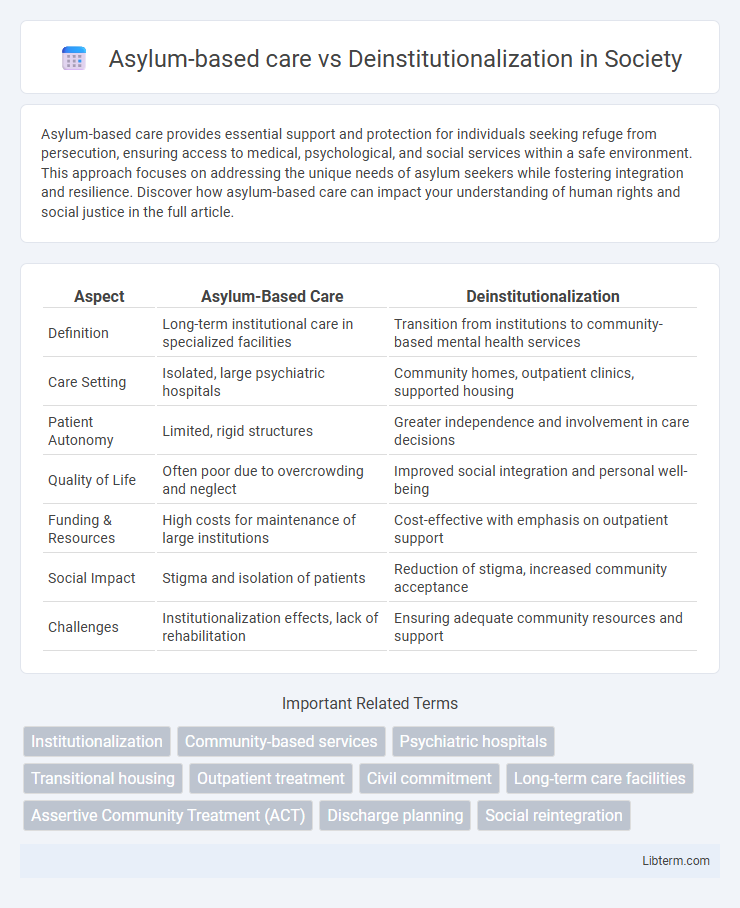
| Aspect | Asylum-Based Care | Deinstitutionalization |
|---|---|---|
| Definition | Long-term institutional care in specialized facilities | Transition from institutions to community-based mental health services |
| Care Setting | Isolated, large psychiatric hospitals | Community homes, outpatient clinics, supported housing |
| Patient Autonomy | Limited, rigid structures | Greater independence and involvement in care decisions |
| Quality of Life | Often poor due to overcrowding and neglect | Improved social integration and personal well-being |
| Funding & Resources | High costs for maintenance of large institutions | Cost-effective with emphasis on outpatient support |
| Social Impact | Stigma and isolation of patients | Reduction of stigma, increased community acceptance |
| Challenges | Institutionalization effects, lack of rehabilitation | Ensuring adequate community resources and support |
Introduction to Mental Health Care Models
Asylum-based care historically centralized treatment for severe mental illnesses within large, often isolated institutions, emphasizing custodial care over therapeutic intervention. Deinstitutionalization shifted the focus to community-based services, aiming to integrate individuals with mental health conditions into society through outpatient treatment and supportive housing. This transition reflects evolving mental health care models prioritizing patient autonomy, social inclusion, and multidisciplinary approaches.
Defining Asylum-Based Care
Asylum-based care refers to a model of mental health treatment where individuals with psychiatric disorders are housed in large, institutional facilities designed for long-term residential care and protection. This system prioritizes containment, structured routines, and medical oversight within often isolated, hospital-like settings to manage severe mental illnesses. In contrast, deinstitutionalization emphasizes transitioning patients to community-based services, aiming to integrate them into society with outpatient support rather than prolonged institutionalization.
Understanding Deinstitutionalization
Deinstitutionalization refers to the systematic process of reducing reliance on large psychiatric hospitals and moving mental health care to community-based settings. This approach emphasizes integrating individuals with mental illnesses into society by providing support through outpatient services, group homes, and local mental health centers. Understanding deinstitutionalization involves recognizing its goals to improve quality of life, enhance social inclusion, and reduce the stigma associated with institutional care.
Historical Evolution of Mental Health Treatment
Asylum-based care dominated the 19th and early 20th centuries, emphasizing long-term institutionalization as the primary treatment method for severe mental illnesses. The mid-20th century shift to deinstitutionalization marked a significant transformation, advocating for community-based care and integration of patients into society through outpatient services and supportive housing. This evolution reflects changes in psychiatric research, drug development, and human rights perspectives influencing mental health policies worldwide.
Benefits of Asylum-Based Care
Asylum-based care provides structured environments with specialized medical and psychological support tailored to severe mental health conditions, ensuring continuous monitoring and crisis intervention. This model facilitates multidisciplinary treatment approaches and guarantees patient safety through secure facilities designed for intensive care. Access to comprehensive resources and trained staff enhances recovery outcomes compared to community-based alternatives.
Advantages of Deinstitutionalization
Deinstitutionalization offers significant advantages such as promoting community integration and improving the quality of life for individuals with mental health conditions. It reduces reliance on large psychiatric institutions by providing personalized, outpatient care that supports autonomy and social inclusion. This approach also decreases stigma and encourages access to diverse support services, enhancing overall mental health outcomes.
Drawbacks and Criticisms of Asylums
Asylum-based care often faced criticism for overcrowding, inadequate treatment, and loss of patient autonomy, leading to neglect and human rights abuses. The institutional environment frequently resulted in social isolation and stigmatization, impairing long-term recovery and integration. These drawbacks prompted the shift towards deinstitutionalization, which emphasized community-based services and personalized care.
Challenges of Deinstitutionalization
Deinstitutionalization, aimed at moving patients from large psychiatric hospitals to community-based care, faces significant challenges such as inadequate funding, limited access to mental health services, and fragmented care coordination. The reduction of institutional beds without sufficient community support often leads to increased homelessness and incarceration of individuals with mental illness. Overcoming these obstacles requires integrated policies, expanded outpatient services, and robust social support systems to ensure effective community reintegration.
Impact on Patients and Communities
Asylum-based care often resulted in patient isolation, limited social integration, and dependency on institutional support, negatively affecting mental health recovery and community reintegration. Deinstitutionalization shifted treatment to community-based services, enhancing patient autonomy, social inclusion, and access to personalized care but challenged communities to provide adequate resources and support systems. The transition significantly influenced mental health outcomes by promoting normalization yet exposed gaps in community infrastructure, impacting both patients' quality of life and the social fabric of affected neighborhoods.
Future Directions in Mental Health Care
Future directions in mental health care emphasize integrating personalized, community-based services to replace traditional asylum-based care and fully realize the goals of deinstitutionalization. Advancements in telepsychiatry and digital health tools enable continuous support, promoting patient autonomy and reducing reliance on institutional settings. Emphasizing trauma-informed care and social determinants of health ensures holistic treatment strategies that improve long-term outcomes for individuals with mental illnesses.
Asylum-based care Infographic
 libterm.com
libterm.com