Disease impacts your body's normal functions and can range from mild to severe conditions affecting overall health. Understanding symptoms, causes, and treatments is crucial for effective management and recovery. Explore the full article to learn how to recognize, prevent, and manage various diseases for better well-being.
Table of Comparison
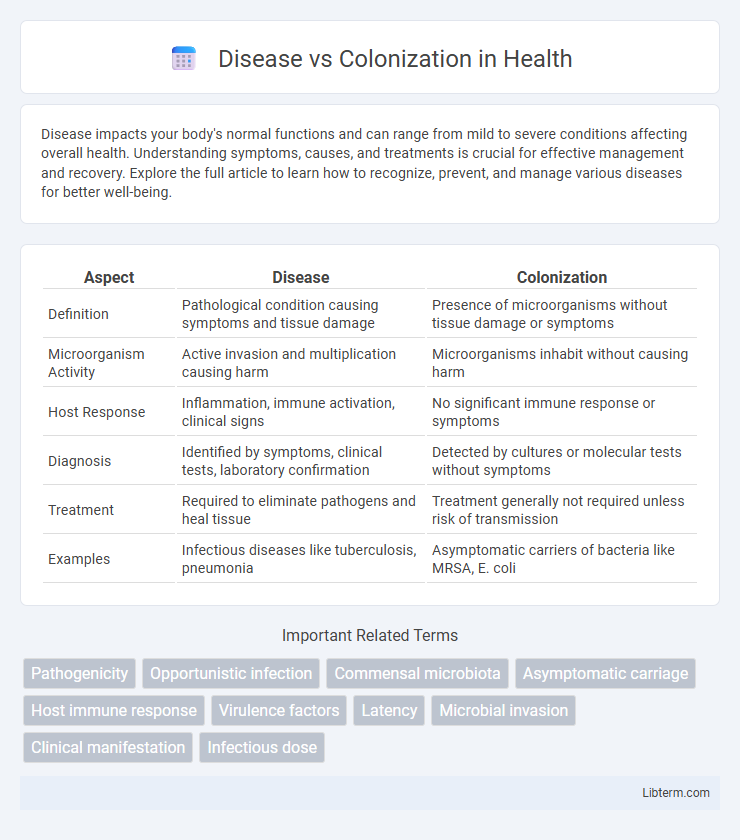
| Aspect | Disease | Colonization |
|---|---|---|
| Definition | Pathological condition causing symptoms and tissue damage | Presence of microorganisms without tissue damage or symptoms |
| Microorganism Activity | Active invasion and multiplication causing harm | Microorganisms inhabit without causing harm |
| Host Response | Inflammation, immune activation, clinical signs | No significant immune response or symptoms |
| Diagnosis | Identified by symptoms, clinical tests, laboratory confirmation | Detected by cultures or molecular tests without symptoms |
| Treatment | Required to eliminate pathogens and heal tissue | Treatment generally not required unless risk of transmission |
| Examples | Infectious diseases like tuberculosis, pneumonia | Asymptomatic carriers of bacteria like MRSA, E. coli |
Defining Disease: Key Concepts and Criteria
Disease is defined by the presence of clinical symptoms and pathological changes resulting from an infection or abnormal condition, whereas colonization refers to the presence of microorganisms without causing harm or symptoms. Key criteria for defining disease include tissue damage, immune response activation, and functional impairment in the host. Differentiating disease from colonization is essential for accurate diagnosis, treatment decisions, and understanding pathogen-host interactions.
Understanding Colonization: A Microbial Perspective
Colonization refers to the presence and growth of microbes on or within a host without causing disease symptoms, representing a stable microbial community. Understanding colonization involves analyzing the interactions between host immune defenses and microbial factors that allow microbes to persist without triggering an inflammatory response. This microbial perspective highlights the importance of distinguishing harmless microbial colonizers from pathogenic organisms to prevent unnecessary treatments and maintain host-microbe homeostasis.
Pathogenesis: How Diseases Develop
Disease development involves the invasion and multiplication of pathogenic microorganisms that disrupt normal tissue function, triggering host immune responses and clinical symptoms. Colonization occurs when microorganisms establish themselves on host surfaces without causing damage or eliciting a significant immune reaction. The transition from colonization to disease depends on factors like microbial virulence, host immune status, and environmental conditions that facilitate pathogen invasion and tissue damage.
Colonization Without Infection: What It Means
Colonization without infection refers to the presence of microorganisms on or within the body without causing tissue damage or clinical symptoms, distinguishing it from active disease. This state often involves bacteria like Staphylococcus aureus or Clostridium difficile residing harmlessly on skin or mucosal surfaces. Understanding colonization is critical for infection control, as these organisms can serve as reservoirs for transmission and potential future infections if host defenses weaken.
Host-Microbe Interactions: Disease vs Colonization
Host-microbe interactions differ fundamentally between disease and colonization, where colonization involves benign coexistence of microbes on or within a host without causing harm, often contributing to important physiological functions such as immune modulation and nutrient synthesis. In contrast, disease arises when microbial pathogenicity factors overcome host defenses, leading to tissue damage, inflammation, and clinical symptoms. Understanding the molecular and immunological mechanisms governing these outcomes is crucial for developing targeted therapies and managing infectious diseases effectively.
Diagnostic Tools: Differentiating Disease from Colonization
Diagnostic tools such as polymerase chain reaction (PCR), quantitative cultures, and biomarker assays are essential in differentiating disease from colonization by detecting microbial load and host response indicators. Advanced imaging techniques like chest X-rays and CT scans help identify structural changes consistent with active infection rather than mere colonization. Combining molecular diagnostics with clinical criteria enhances accuracy in distinguishing pathogenic infection from harmless microbial presence.
Clinical Manifestations: Signs of True Disease
Clinical manifestations of true disease typically include pronounced symptoms such as fever, localized pain, inflammation, purulent discharge, and tissue damage, distinguishing it from mere colonization. Unlike asymptomatic colonization where microbes reside without causing harm, true disease presents with systemic signs like elevated white blood cell counts, increased inflammatory markers, and evidence of organ dysfunction. Accurate identification of these signs is crucial for effective diagnosis and treatment, preventing progression to severe complications or chronic infection.
Risk Factors Influencing Colonization and Disease
Risk factors influencing colonization and disease include host immune status, genetic predispositions, and environmental exposures such as antibiotic use and hygiene practices. Pathogen virulence, including bacterial adhesins and toxins, plays a crucial role in transitioning from asymptomatic colonization to active infection. Medical devices, comorbidities like diabetes, and hospital settings increase susceptibility to colonization progressing into disease.
Treatment Approaches: Managing Colonization vs Disease
Treatment approaches differ significantly between colonization and disease; colonization often requires monitoring without antibiotics to prevent resistance, while disease necessitates targeted antimicrobial therapy based on pathogen identification and susceptibility. Managing colonization involves infection control measures, such as hygiene and isolation protocols, to prevent progression to disease and transmission. In contrast, disease management focuses on symptomatic relief, eliminating the infectious agent, and addressing complications through appropriate drug regimens and supportive care.
Public Health Implications: Why the Distinction Matters
Distinguishing disease from colonization is crucial for public health strategies, as disease involves active infection causing symptoms and potential transmission risks, while colonization refers to the presence of microorganisms without causing harm. Misinterpreting colonization as disease can lead to unnecessary antibiotic use, increasing resistance and complicating infection control efforts. Accurate identification informs targeted interventions, resource allocation, and surveillance, ultimately reducing the burden of infectious diseases in communities.
Disease Infographic
 libterm.com
libterm.com