Lithiasis often leads to the formation of stones within the urinary tract, causing obstruction and increasing the risk of infection due to stagnant urine and bacterial growth. Persistent infections can exacerbate stone formation, creating a cycle that complicates treatment and patient outcomes. Explore the rest of the article to understand effective strategies for managing lithiasis and preventing associated infections.
Table of Comparison
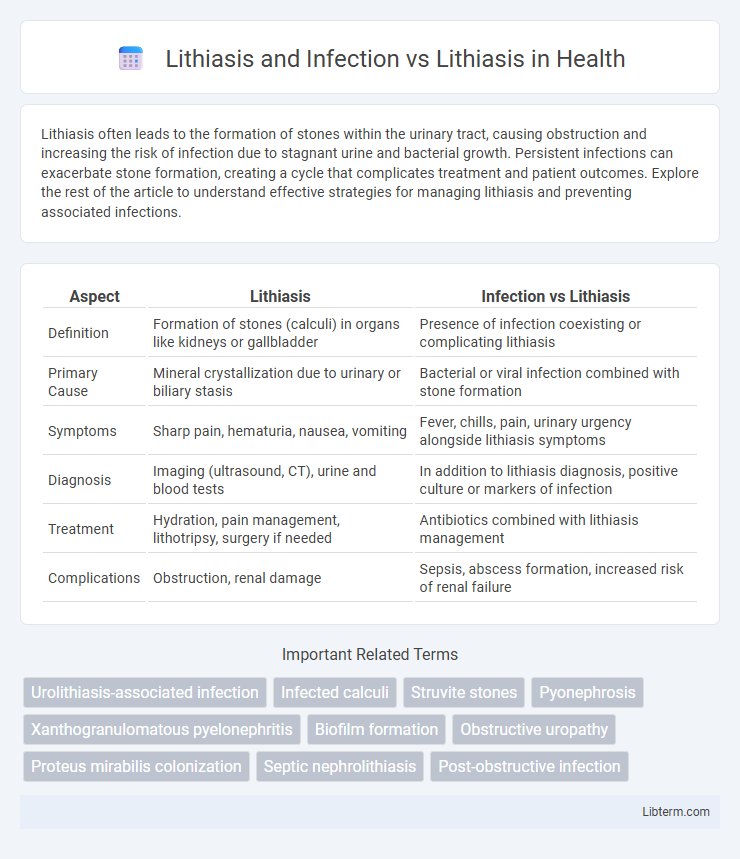
| Aspect | Lithiasis | Infection vs Lithiasis |
|---|---|---|
| Definition | Formation of stones (calculi) in organs like kidneys or gallbladder | Presence of infection coexisting or complicating lithiasis |
| Primary Cause | Mineral crystallization due to urinary or biliary stasis | Bacterial or viral infection combined with stone formation |
| Symptoms | Sharp pain, hematuria, nausea, vomiting | Fever, chills, pain, urinary urgency alongside lithiasis symptoms |
| Diagnosis | Imaging (ultrasound, CT), urine and blood tests | In addition to lithiasis diagnosis, positive culture or markers of infection |
| Treatment | Hydration, pain management, lithotripsy, surgery if needed | Antibiotics combined with lithiasis management |
| Complications | Obstruction, renal damage | Sepsis, abscess formation, increased risk of renal failure |
Understanding Lithiasis: Definition and Types
Lithiasis refers to the formation of stones, or calculi, in the urinary or biliary tract, with major types including kidney stones (renal lithiasis) and gallstones (cholelithiasis). Infection-related lithiasis involves the presence of bacteria that promote stone formation, often resulting in struvite stones linked to urinary tract infections. Understanding the distinctions between infection-associated lithiasis and non-infectious lithiasis aids in diagnosis, treatment decisions, and prevention strategies.
Pathophysiology of Lithiasis Formation
Lithiasis formation primarily results from supersaturation of urine with stone-forming salts such as calcium, oxalate, and uric acid, leading to crystal nucleation and aggregation within the renal tubules. Infection-related lithiasis involves urease-producing bacteria that alkalinize urine, promoting struvite stone formation through precipitation of magnesium ammonium phosphate. Non-infectious lithiasis arises from metabolic imbalances, dehydration, or genetic predispositions that alter urinary pH and solute concentration, facilitating stone pathophysiology distinct from infection-mediated mechanisms.
Common Causes and Risk Factors for Lithiasis
Lithiasis, commonly caused by factors such as dehydration, high dietary oxalate intake, obesity, and metabolic disorders like hyperparathyroidism, results in the formation of stones within the urinary tract. Infection-induced lithiasis often arises from urease-producing bacteria like Proteus mirabilis, leading to struvite stone formation. Risk factors for lithiasis include genetic predisposition, recurrent urinary tract infections, low fluid intake, and certain anatomical abnormalities that promote stone retention and growth.
Lithiasis Without Infection: Clinical Presentation
Lithiasis without infection typically presents with asymptomatic or mild symptoms such as intermittent flank pain and hematuria, often detected incidentally during imaging studies. Patients may experience discomfort due to urinary tract obstruction caused by calculi but lack systemic signs of infection like fever or leukocytosis. Radiological evaluations, including ultrasound or CT scans, are essential for diagnosing non-infectious lithiasis and guiding appropriate management strategies.
Role of Infection in Lithiasis Development
Infection plays a significant role in the development of certain types of lithiasis, particularly struvite stones, which are directly linked to urinary tract infections caused by urease-producing bacteria such as Proteus mirabilis. These infections increase urine pH and promote the precipitation of magnesium ammonium phosphate crystals, leading to stone formation. Understanding the microbial contribution to lithiasis is essential for targeted prevention and treatment strategies.
Lithiasis and Infection: Pathogenic Interactions
Lithiasis and infection interact through complex pathogenic mechanisms where stones provide a nidus for bacterial colonization, leading to persistent urinary infections. The biofilm formed on lithiasis surfaces protects pathogens from host defenses and antibiotics, exacerbating inflammation and tissue damage. This interplay increases the risk of recurrent infections and complicates treatment strategies for both conditions.
Diagnostic Approaches: Lithiasis vs Lithiasis with Infection
Diagnostic approaches for lithiasis focus on imaging techniques such as ultrasound, X-rays, and CT scans to detect calculi and assess their size and location. In cases of lithiasis with infection, laboratory tests including urinalysis, urine culture, and blood tests for inflammatory markers are crucial to identify bacterial presence and systemic infection. Combining imaging with microbiological analysis ensures accurate diagnosis and guides appropriate treatment strategies.
Treatment Strategies: Managing Lithiasis Alone
Managing lithiasis alone focuses on non-invasive methods such as hydration therapy, pain management, and pharmacological agents like alpha-blockers to facilitate stone passage. Extracorporeal shock wave lithotripsy (ESWL) and ureteroscopy are common minimally invasive procedures for stones that do not pass spontaneously. Tailoring treatment to stone size, location, and composition optimizes outcomes while minimizing complications and preserving renal function.
Treatment Strategies: Managing Lithiasis with Infection
Managing lithiasis with infection requires prompt antibiotic therapy combined with urgent stone removal to prevent sepsis and preserve renal function. Ureteral stenting or percutaneous nephrostomy facilitates drainage of infected urine, while definitive treatment includes extracorporeal shock wave lithotripsy (ESWL) or ureteroscopy once infection is controlled. In contrast, lithiasis without infection often allows elective stone removal focusing on pain management and lithotripsy without immediate drainage.
Prognosis and Prevention: Importance of Infection Control in Lithiasis
Lithiasis complicated by infection presents a more severe prognosis due to risks of sepsis and renal damage, necessitating urgent intervention to prevent life-threatening outcomes. Infection control in lithiasis involves timely antibiotic therapy and sterile techniques during stone removal to reduce recurrence and complications. Preventive strategies focus on maintaining urinary tract sterility, hydration, and treating underlying infections to improve long-term outcomes and reduce the likelihood of chronic kidney disease.
Lithiasis and Infection Infographic
 libterm.com
libterm.com