Inflammatory responses are the body's natural reaction to injury or infection, aiming to eliminate harmful stimuli and initiate healing. Chronic inflammation, however, can contribute to various diseases such as arthritis, heart disease, and diabetes. Discover how understanding the causes and management of inflammation can improve Your overall health in the rest of this article.
Table of Comparison
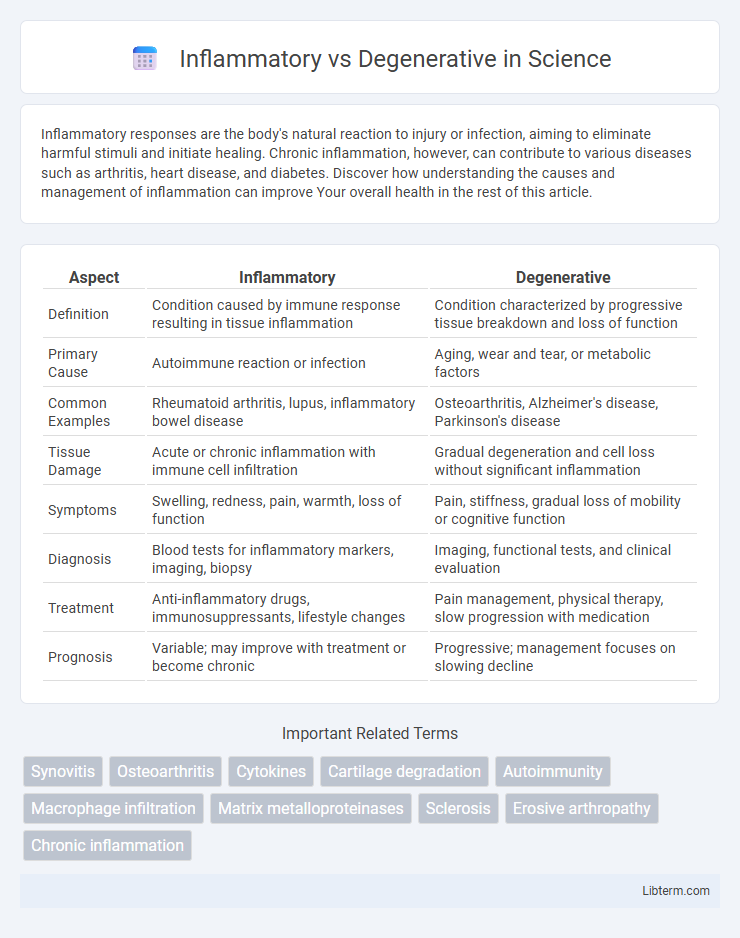
| Aspect | Inflammatory | Degenerative |
|---|---|---|
| Definition | Condition caused by immune response resulting in tissue inflammation | Condition characterized by progressive tissue breakdown and loss of function |
| Primary Cause | Autoimmune reaction or infection | Aging, wear and tear, or metabolic factors |
| Common Examples | Rheumatoid arthritis, lupus, inflammatory bowel disease | Osteoarthritis, Alzheimer's disease, Parkinson's disease |
| Tissue Damage | Acute or chronic inflammation with immune cell infiltration | Gradual degeneration and cell loss without significant inflammation |
| Symptoms | Swelling, redness, pain, warmth, loss of function | Pain, stiffness, gradual loss of mobility or cognitive function |
| Diagnosis | Blood tests for inflammatory markers, imaging, biopsy | Imaging, functional tests, and clinical evaluation |
| Treatment | Anti-inflammatory drugs, immunosuppressants, lifestyle changes | Pain management, physical therapy, slow progression with medication |
| Prognosis | Variable; may improve with treatment or become chronic | Progressive; management focuses on slowing decline |
Understanding Inflammatory and Degenerative Disorders
Inflammatory disorders involve immune system activation causing tissue inflammation, pain, and swelling, as seen in rheumatoid arthritis, whereas degenerative disorders result from progressive tissue deterioration, such as osteoarthritis and Alzheimer's disease. Understanding the distinct pathological mechanisms, including immune response in inflammatory diseases and cellular degradation in degenerative conditions, is crucial for accurate diagnosis and effective treatment strategies. Biomarkers like C-reactive protein (CRP) indicate inflammation, while imaging techniques assess structural degeneration, guiding personalized medical interventions.
Key Differences Between Inflammatory and Degenerative Conditions
Inflammatory conditions involve the immune system attacking tissues, causing redness, swelling, and pain, while degenerative conditions result from wear and tear or aging, leading to gradual tissue breakdown and loss of function. Inflammatory diseases, such as rheumatoid arthritis, often present with systemic symptoms like fever and fatigue, whereas degenerative diseases, like osteoarthritis, primarily cause localized joint stiffness and reduced mobility. Diagnostic markers like elevated C-reactive protein and erythrocyte sedimentation rate are common in inflammatory conditions but typically absent in degenerative disorders.
Common Causes: Inflammation vs. Degeneration
Inflammatory conditions are commonly caused by infections, autoimmune disorders, and exposure to irritants that trigger an immune response, leading to tissue swelling and pain. Degenerative diseases primarily result from aging, wear and tear, and chronic mechanical stress, causing deterioration of cartilage, joints, and tissues over time. Understanding the different etiologies is crucial for targeted treatments in conditions like rheumatoid arthritis versus osteoarthritis.
Symptoms Comparison: Inflammatory vs. Degenerative Diseases
Inflammatory diseases often present with acute symptoms such as swelling, redness, warmth, and severe pain due to immune system activation, whereas degenerative diseases typically exhibit chronic, progressive symptoms like joint stiffness, reduced mobility, and gradual pain increase. Morning stiffness lasting less than 30 minutes is common in degenerative osteoarthritis, while inflammatory conditions like rheumatoid arthritis cause prolonged morning stiffness exceeding an hour. Systemic symptoms such as fever and fatigue are more characteristic of inflammatory diseases and rarely appear in purely degenerative disorders.
Diagnostic Tools for Differentiating Disease Types
Diagnostic tools for differentiating inflammatory versus degenerative diseases include MRI, which highlights inflammation through contrast enhancement and edema, while degenerative changes appear as cartilage loss and bone spurs. Blood tests measuring inflammatory markers like ESR and CRP help identify systemic inflammation typical of inflammatory diseases but are usually normal in degenerative conditions. Joint fluid analysis further distinguishes between infectious or autoimmune inflammation and non-inflammatory degenerative joint disease by assessing cell count and presence of crystals or pathogens.
Treatment Approaches: Inflammatory vs. Degenerative
Inflammatory conditions often require immunosuppressive or anti-inflammatory medications such as corticosteroids and disease-modifying antirheumatic drugs (DMARDs) to reduce immune system activity and control inflammation. Degenerative diseases primarily focus on symptom management through physical therapy, pain relief medications like NSAIDs, and lifestyle modifications to slow progression and improve joint function. Advanced cases of degenerative disorders may involve surgical interventions such as joint replacement, while inflammatory diseases might require biological therapies targeting specific immune pathways.
Role of Immune System in Inflammatory Diseases
The immune system plays a central role in inflammatory diseases by triggering an exaggerated response against pathogens or self-antigens, leading to tissue inflammation and damage. Inflammatory diseases like rheumatoid arthritis and lupus involve immune cells such as T cells, B cells, and cytokines that perpetuate chronic inflammation. In contrast, degenerative diseases primarily result from wear and tear or cellular aging without significant immune system activation.
Age-Related Factors in Degenerative Disorders
Degenerative disorders often result from age-related factors such as the progressive loss of cellular function, accumulation of oxidative damage, and reduced regenerative capacity in tissues. Inflammatory conditions, by contrast, primarily involve immune system activation and tissue inflammation, but do not necessarily correlate with aging processes. Age-related degeneration is commonly observed in diseases like osteoarthritis, Alzheimer's, and macular degeneration, where chronic wear and neuronal loss worsen over time.
Prevention Strategies for Both Conditions
Inflammatory conditions like rheumatoid arthritis require early intervention with anti-inflammatory diets rich in omega-3 fatty acids and regular low-impact exercise to reduce joint inflammation and prevent tissue damage. Degenerative diseases such as osteoarthritis benefit from maintaining a healthy weight, engaging in strength training to support joint stability, and avoiding repetitive joint stress to slow cartilage breakdown. Both conditions respond well to lifestyle modifications that promote joint health and minimize symptom progression, emphasizing tailored physical therapy regimens and balanced nutrition.
Prognosis and Long-Term Management
Inflammatory conditions, such as rheumatoid arthritis, often respond well to early aggressive immunosuppressive treatment, improving long-term prognosis by preventing joint damage and maintaining function. Degenerative disorders like osteoarthritis typically have a slower progression with management centered on symptom control, physical therapy, and lifestyle modifications to delay further joint deterioration. Long-term management for inflammatory diseases requires consistent monitoring for flare-ups and medication side effects, whereas degenerative diseases prioritize pain management and mobility preservation.
Inflammatory Infographic
 libterm.com
libterm.com