Hypoperfusion occurs when there is inadequate blood flow to tissues and organs, leading to insufficient oxygen and nutrient delivery essential for cellular function. This condition can result from various causes such as shock, heart failure, or vascular obstruction, and requires prompt diagnosis to prevent tissue damage or organ failure. Explore this article to understand the causes, symptoms, and treatment options to protect your health effectively.
Table of Comparison
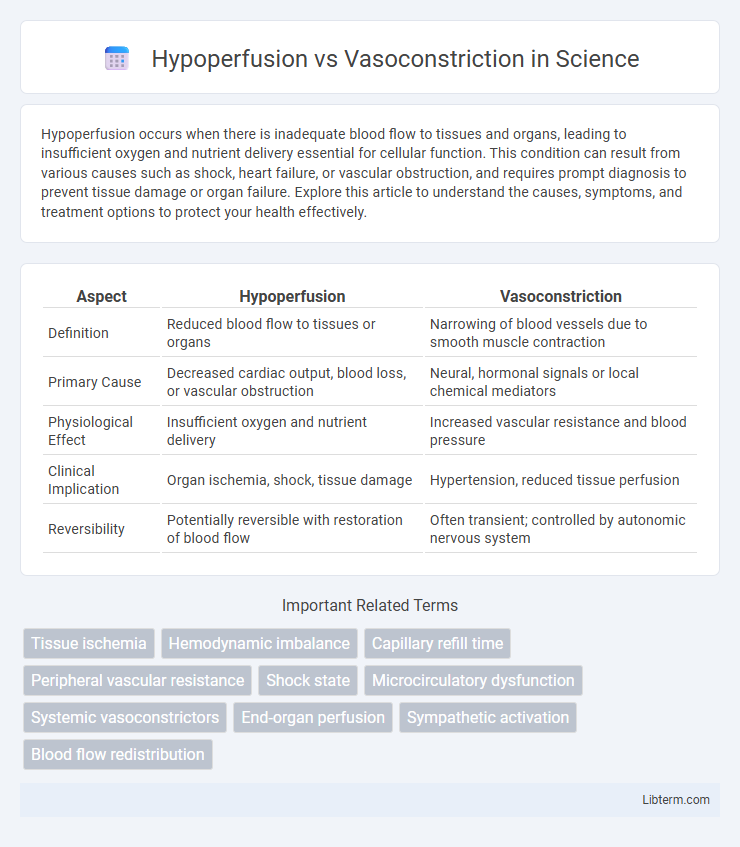
| Aspect | Hypoperfusion | Vasoconstriction |
|---|---|---|
| Definition | Reduced blood flow to tissues or organs | Narrowing of blood vessels due to smooth muscle contraction |
| Primary Cause | Decreased cardiac output, blood loss, or vascular obstruction | Neural, hormonal signals or local chemical mediators |
| Physiological Effect | Insufficient oxygen and nutrient delivery | Increased vascular resistance and blood pressure |
| Clinical Implication | Organ ischemia, shock, tissue damage | Hypertension, reduced tissue perfusion |
| Reversibility | Potentially reversible with restoration of blood flow | Often transient; controlled by autonomic nervous system |
Introduction to Hypoperfusion and Vasoconstriction
Hypoperfusion refers to inadequate blood flow to tissues, resulting in insufficient oxygen and nutrient delivery necessary for cellular metabolism. Vasoconstriction involves the narrowing of blood vessels due to the contraction of muscular walls, often triggered by physiological or pathological stimuli to regulate blood pressure and flow. Understanding the mechanisms and effects of hypoperfusion and vasoconstriction is crucial in diagnosing and managing cardiovascular and systemic conditions.
Defining Hypoperfusion: Causes and Mechanisms
Hypoperfusion occurs when there is an inadequate blood flow to tissues, resulting in insufficient oxygen and nutrient delivery, often caused by shock, cardiac failure, or severe blood loss. The primary mechanisms involve reduced cardiac output, vascular obstruction, or blood volume depletion, leading to compromised microcirculation and cellular hypoxia. Understanding hypoperfusion is crucial in distinguishing it from vasoconstriction, which involves narrowing of blood vessels but does not necessarily reduce overall blood flow to the same extent.
Understanding Vasoconstriction: Key Triggers
Vasoconstriction is primarily triggered by factors such as cold temperatures, stress-induced sympathetic nervous system activation, and the release of vasoconstrictive substances like norepinephrine and angiotensin II. This process reduces blood vessel diameter, increasing vascular resistance and affecting tissue perfusion. Understanding these triggers is crucial for distinguishing vasoconstriction from hypoperfusion, which involves reduced blood flow due to other causes like hypovolemia or cardiac dysfunction.
Pathophysiological Differences
Hypoperfusion refers to an inadequate blood flow to tissues, leading to oxygen and nutrient deprivation caused by factors like shock or heart failure, whereas vasoconstriction involves the narrowing of blood vessels due to smooth muscle contraction, increasing vascular resistance and blood pressure. In hypoperfusion, tissue ischemia results primarily from insufficient perfusion pressure or volume, while vasoconstriction aims to regulate blood distribution and maintain systemic vascular resistance under physiological or pathological conditions. The pathophysiological difference lies in hypoperfusion being a result of reduced blood supply causing cellular hypoxia, whereas vasoconstriction is a compensatory mechanism that may exacerbate hypoperfusion by limiting downstream blood flow.
Clinical Manifestations: Comparing Symptoms
Hypoperfusion typically presents with symptoms such as hypotension, altered mental status, cold clammy skin, and tachycardia due to inadequate tissue perfusion. In contrast, vasoconstriction often manifests through localized symptoms like pallor, cyanosis, and cold extremities caused by reduced blood flow to specific areas. Both conditions can lead to tissue hypoxia, but hypoperfusion generally affects systemic circulation, while vasoconstriction is more focused on regional blood flow abnormalities.
Diagnostic Approaches for Hypoperfusion and Vasoconstriction
Diagnostic approaches for hypoperfusion involve measuring tissue oxygenation and blood flow using techniques such as near-infrared spectroscopy (NIRS), Doppler ultrasound, and lactate level assessment to detect inadequate perfusion. Vasoconstriction is primarily evaluated through imaging modalities like angiography and laser Doppler flowmetry, as well as by assessing systemic vascular resistance and endothelial function using biomarkers and non-invasive blood pressure monitoring. Distinguishing hypoperfusion from vasoconstriction requires integrating hemodynamic data, biochemical markers, and microcirculatory imaging to tailor targeted therapeutic interventions.
Impact on Organ Systems
Hypoperfusion reduces oxygen and nutrient delivery to organs, leading to cellular dysfunction and tissue damage, particularly in the brain, kidneys, and heart. Vasoconstriction increases vascular resistance, causing elevated blood pressure and potentially reducing blood flow to peripheral tissues, which can exacerbate ischemic conditions. Both mechanisms disrupt homeostasis but differ in their hemodynamic effects and resultant organ system impairments.
Treatment Strategies: Hypoperfusion vs Vasoconstriction
Treatment strategies for hypoperfusion prioritize restoring adequate blood flow through volume resuscitation and vasodilators to improve tissue oxygenation. In contrast, vasoconstriction treatment focuses on modulating vessel tone using vasodilators or specific receptor blockers to reduce excessive narrowing and enhance perfusion. Targeted therapies depend on identifying the underlying cause, such as fluid replacement for hypovolemia-induced hypoperfusion versus pharmacologic agents for pathologic vasoconstriction.
Prognosis and Patient Outcomes
Hypoperfusion often leads to tissue ischemia and organ dysfunction, resulting in poorer patient outcomes and higher mortality rates if not promptly managed. Vasoconstriction, while potentially beneficial in maintaining blood pressure during shock states, can exacerbate hypoperfusion by reducing microcirculatory blood flow, negatively impacting prognosis. Effective treatment strategies targeting both hypoperfusion and pathologic vasoconstriction significantly improve survival rates and functional recovery in critical care settings.
Summary: Key Takeaways and Future Perspectives
Hypoperfusion involves inadequate blood flow leading to tissue ischemia, while vasoconstriction refers to the narrowing of blood vessels that can exacerbate or result from hypoperfusion. Understanding the interplay between these mechanisms is crucial for developing targeted therapies in conditions like shock and cardiovascular diseases. Future research aims to better elucidate molecular pathways governing vascular tone and tissue perfusion to improve clinical interventions and patient outcomes.
Hypoperfusion Infographic
 libterm.com
libterm.com