Institutionalization refers to the process by which individuals become embedded within established systems or organizations, often leading to routine behaviors and norms that shape their actions and identity. It plays a crucial role in social structures, ensuring stability and continuity through formal rules and regulations. Explore the rest of the article to understand how institutionalization impacts various aspects of society and your interactions within these frameworks.
Table of Comparison
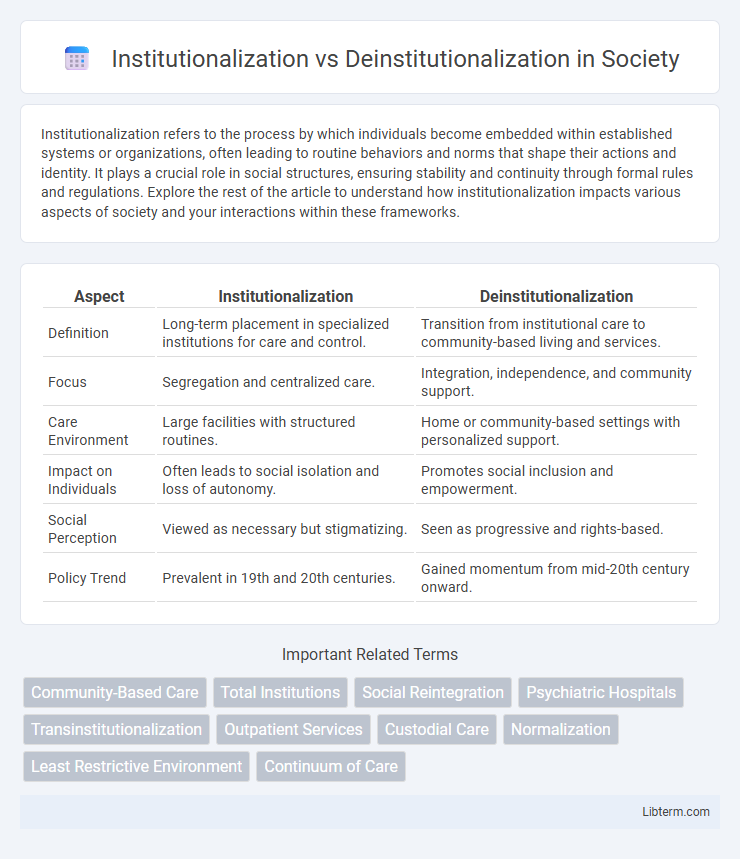
| Aspect | Institutionalization | Deinstitutionalization |
|---|---|---|
| Definition | Long-term placement in specialized institutions for care and control. | Transition from institutional care to community-based living and services. |
| Focus | Segregation and centralized care. | Integration, independence, and community support. |
| Care Environment | Large facilities with structured routines. | Home or community-based settings with personalized support. |
| Impact on Individuals | Often leads to social isolation and loss of autonomy. | Promotes social inclusion and empowerment. |
| Social Perception | Viewed as necessary but stigmatizing. | Seen as progressive and rights-based. |
| Policy Trend | Prevalent in 19th and 20th centuries. | Gained momentum from mid-20th century onward. |
Introduction to Institutionalization and Deinstitutionalization
Institutionalization refers to the practice of placing individuals with mental health disorders or disabilities into long-term residential facilities, often leading to segregation from society. Deinstitutionalization emerged as a movement advocating the transition from these large institutions to community-based care, emphasizing integration, independence, and improved quality of life. This shift has been driven by advances in psychiatric treatments, human rights considerations, and the development of outpatient support systems.
Historical Overview of Institutional Care
Institutional care emerged in the 18th and 19th centuries as a response to social issues such as mental illness, poverty, and disability, characterized by large asylums and custodial care models. The mid-20th century witnessed a significant shift toward deinstitutionalization, driven by advancements in psychiatric medication, changing social attitudes, and policy reforms promoting community-based services. This historical transition reflects evolving perspectives on human rights and the effectiveness of care, emphasizing rehabilitation and integration rather than segregation and confinement.
Origins and Philosophy of Deinstitutionalization
Deinstitutionalization emerged in the mid-20th century as a response to the widespread use of large psychiatric institutions, aiming to shift mental health care from isolated hospitals to community-based services. Rooted in humanistic philosophy and civil rights movements, it emphasized the empowerment, dignity, and integration of individuals with mental illnesses into society. This approach challenged the traditional institutional model by advocating for outpatient treatment, personalized care, and social support systems as more effective and humane alternatives.
Key Differences Between Institutionalization and Deinstitutionalization
Institutionalization involves placing individuals in structured, long-term care facilities designed to provide comprehensive support and supervision, often limiting personal autonomy. Deinstitutionalization shifts focus toward community-based services and integration, emphasizing independence, social inclusion, and personalized care plans outside of institutional settings. Key differences include the level of autonomy, care environment, and the emphasis on self-determination versus structured supervision.
Social and Psychological Impacts of Institutionalization
Institutionalization often leads to social isolation, impairing an individual's ability to form meaningful relationships due to restricted social interactions and rigid routines. Psychologically, prolonged institutional care can result in learned helplessness, lowered self-esteem, and increased dependency, hindering personal autonomy and mental well-being. These impacts contrast sharply with deinstitutionalization, which aims to promote social integration and psychological resilience by reintegrating individuals into community settings.
Benefits and Challenges of Deinstitutionalization
Deinstitutionalization promotes community integration and enhances individual autonomy by transitioning people with mental health or developmental conditions from large institutions to less restrictive, community-based settings. Benefits include improved quality of life, increased access to personalized care, and reduced social stigma. Challenges involve ensuring adequate funding for community services, addressing gaps in mental health support, and preventing homelessness or neglect among vulnerable populations.
Case Studies: Successes and Failures in Deinstitutionalization
Case studies on deinstitutionalization reveal varied outcomes, highlighting successes like improved community integration and autonomy for former institutionalized individuals in countries such as Italy and Sweden, where robust community support systems were established. Conversely, failures in nations lacking adequate infrastructure, including parts of the United States and Eastern Europe, demonstrate increased homelessness, incarceration, and insufficient mental health care following institutional closures. These case studies emphasize the critical role of comprehensive planning, continuous funding, and community-based services in achieving successful deinstitutionalization.
Policy and Legal Frameworks Shaping Care Models
Policy and legal frameworks fundamentally influence the shift between institutionalization and deinstitutionalization by determining funding allocations, care standards, and regulatory oversight. Institutional models often rely on laws that sanction long-term confinement and centralized care, while deinstitutionalization is driven by policies promoting community-based services, human rights protections, and inclusive social integration. Legal reforms such as the Americans with Disabilities Act or the Mental Health Act emphasize individual autonomy and mandate accessible support systems, reshaping care models toward less restrictive environments.
Community-Based Alternatives to Institutionalization
Community-based alternatives to institutionalization emphasize personalized care within familiar environments, promoting social integration and independence for individuals with disabilities or mental health conditions. Programs such as supported housing, day centers, and community mental health teams provide tailored support, reducing reliance on large-scale institutions. These alternatives improve quality of life by fostering empowerment, connectivity, and access to localized resources, aligning with human rights standards and modern healthcare practices.
Future Directions: Toward Inclusive Support Systems
Future directions in institutionalization versus deinstitutionalization emphasize the development of inclusive support systems that prioritize community-based care and personalized services. Emerging models integrate technology, such as telehealth and digital monitoring, to enhance autonomy and accessibility for individuals with disabilities or mental health needs. Policy frameworks increasingly advocate for collaborative networks among healthcare providers, social services, and families to ensure sustainable, person-centered support.
Institutionalization Infographic
 libterm.com
libterm.com