Bronchodilators are medications that relax the muscles around the airways, helping to open them up and improve breathing in conditions like asthma and chronic obstructive pulmonary disease (COPD). These drugs can be short-acting for quick relief or long-acting for ongoing control of symptoms. Explore the article to learn how bronchodilators work and which options might be best for your respiratory health.
Table of Comparison
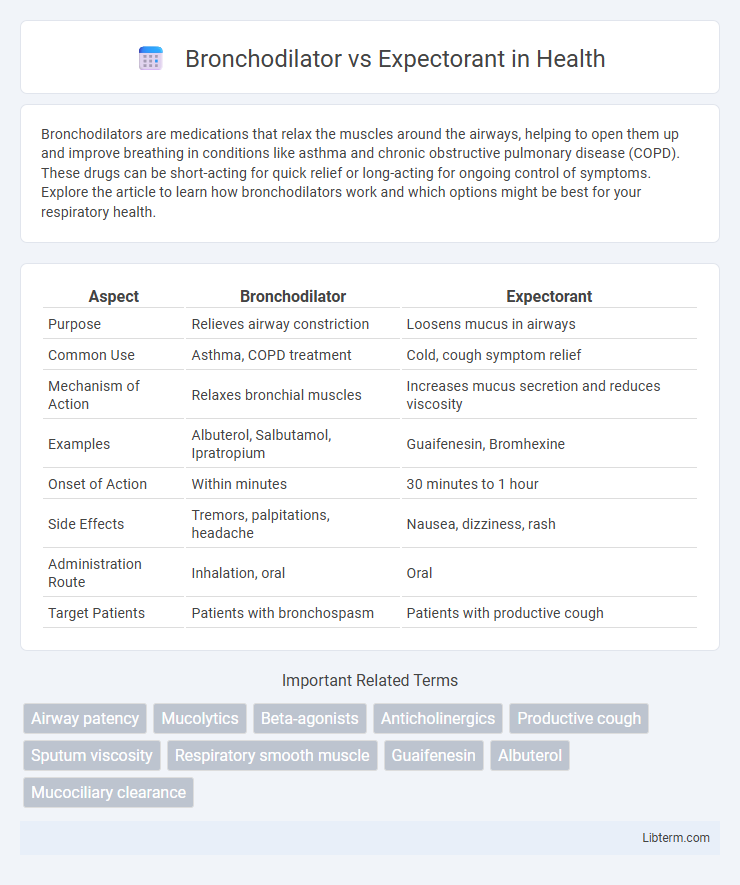
| Aspect | Bronchodilator | Expectorant |
|---|---|---|
| Purpose | Relieves airway constriction | Loosens mucus in airways |
| Common Use | Asthma, COPD treatment | Cold, cough symptom relief |
| Mechanism of Action | Relaxes bronchial muscles | Increases mucus secretion and reduces viscosity |
| Examples | Albuterol, Salbutamol, Ipratropium | Guaifenesin, Bromhexine |
| Onset of Action | Within minutes | 30 minutes to 1 hour |
| Side Effects | Tremors, palpitations, headache | Nausea, dizziness, rash |
| Administration Route | Inhalation, oral | Oral |
| Target Patients | Patients with bronchospasm | Patients with productive cough |
Introduction to Bronchodilators and Expectorants
Bronchodilators are medications that relax the muscles around the airways, improving airflow and easing breathing in conditions like asthma and chronic obstructive pulmonary disease (COPD). Expectorants, such as guaifenesin, work by thinning mucus in the respiratory tract, facilitating its clearance from the lungs and reducing chest congestion. Both bronchodilators and expectorants play complementary roles in respiratory therapy by addressing airway constriction and mucus buildup, respectively.
Understanding Bronchodilators: Mechanism and Uses
Bronchodilators function by relaxing the smooth muscles surrounding the airways, thereby widening the bronchial tubes and facilitating easier airflow to the lungs. Commonly prescribed for conditions such as asthma, chronic obstructive pulmonary disease (COPD), and bronchitis, bronchodilators help alleviate symptoms like wheezing, shortness of breath, and chest tightness. These medications include beta-agonists, anticholinergics, and methylxanthines, each working through distinct mechanisms to open air passages and improve respiratory function.
Expectorants Explained: How They Work
Expectorants enhance respiratory health by thinning mucus in the airways, making it easier to cough up and clear from the lungs. Commonly containing guaifenesin, expectorants increase the hydration of mucus secretions, reducing viscosity and promoting effective clearance. Unlike bronchodilators that relax airway muscles to improve airflow, expectorants specifically target mucus consistency, facilitating better expectoration and relief from chest congestion.
Key Differences Between Bronchodilators and Expectorants
Bronchodilators primarily work by relaxing the muscles around the airways, leading to widened bronchial passages and improved airflow, which is crucial for conditions like asthma and chronic obstructive pulmonary disease (COPD). Expectorants facilitate the clearance of mucus from the respiratory tract by thinning and loosening phlegm, thereby easing cough and congestion in illnesses such as bronchitis and the common cold. The key difference lies in their mechanisms and targets: bronchodilators address airway constriction, while expectorants enhance mucus clearance for respiratory symptom relief.
Common Conditions Treated with Bronchodilators
Bronchodilators are primarily used to treat respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and bronchitis by relaxing the muscles around the airways and improving airflow. Unlike expectorants, which help thin and loosen mucus in the airways for easier coughing, bronchodilators target airway constriction to relieve symptoms like wheezing, shortness of breath, and chest tightness. Common bronchodilators include beta-agonists like albuterol and anticholinergics such as ipratropium, which are essential in managing acute asthma attacks and chronic respiratory diseases.
Typical Applications of Expectorants
Expectorants are commonly used to treat respiratory conditions characterized by thick mucus production, such as bronchitis, chronic obstructive pulmonary disease (COPD), and common colds. These medications work by thinning mucus secretion, making it easier to cough up and clear from the airways. Unlike bronchodilators, which primarily relax airway muscles to improve breathing, expectorants target mucus consistency to enhance mucociliary clearance and reduce chest congestion.
Side Effects and Precautions: Bronchodilators vs Expectorants
Bronchodilators commonly cause side effects such as tremors, palpitations, and increased heart rate, requiring caution in patients with cardiovascular conditions or hypertension. Expectorants may lead to gastrointestinal discomfort and allergic reactions, necessitating careful use in individuals with sensitive digestive systems or known allergies. Both medications should be used under medical supervision to avoid adverse interactions and ensure appropriate treatment based on respiratory condition severity.
Combined Use: Can You Take Both Together?
Bronchodilators and expectorants serve distinct functions in respiratory care, with bronchodilators relaxing airway muscles to improve breathing and expectorants thinning mucus for easier clearance. Using both together can be beneficial for patients who experience bronchospasm accompanied by thick mucus, as this combination helps open airways while facilitating mucus removal. Consultation with a healthcare provider is essential to ensure proper dosing and avoid potential interactions or side effects.
Choosing the Right Treatment for Respiratory Conditions
Bronchodilators relax airway muscles to improve airflow, making them ideal for conditions such as asthma and chronic obstructive pulmonary disease (COPD). Expectorants promote mucus clearance by thinning respiratory secretions, which helps alleviate chest congestion in bronchitis and common colds. Selecting the appropriate treatment depends on the primary symptom--airway constriction warrants bronchodilators, while excessive mucus production calls for expectorants.
When to Consult a Healthcare Professional
Consult a healthcare professional when experiencing persistent wheezing, shortness of breath, or chest tightness that may require bronchodilator therapy to open airways. Seek medical advice if a cough produces thick mucus or lasts more than three weeks, indicating the possible need for an expectorant to clear respiratory secretions. Immediate consultation is essential if symptoms worsen, or if there's difficulty breathing or suspected respiratory infections.
Bronchodilator Infographic
 libterm.com
libterm.com