Gastroparesis and irritable bowel syndrome are digestive disorders that impact gastrointestinal function but differ significantly in symptoms and causes. Gastroparesis involves delayed stomach emptying causing nausea, bloating, and vomiting, while irritable bowel syndrome primarily affects the large intestine with symptoms like abdominal pain, diarrhea, and constipation. Explore the article to understand how these conditions affect your digestive health and discover effective management strategies.
Table of Comparison
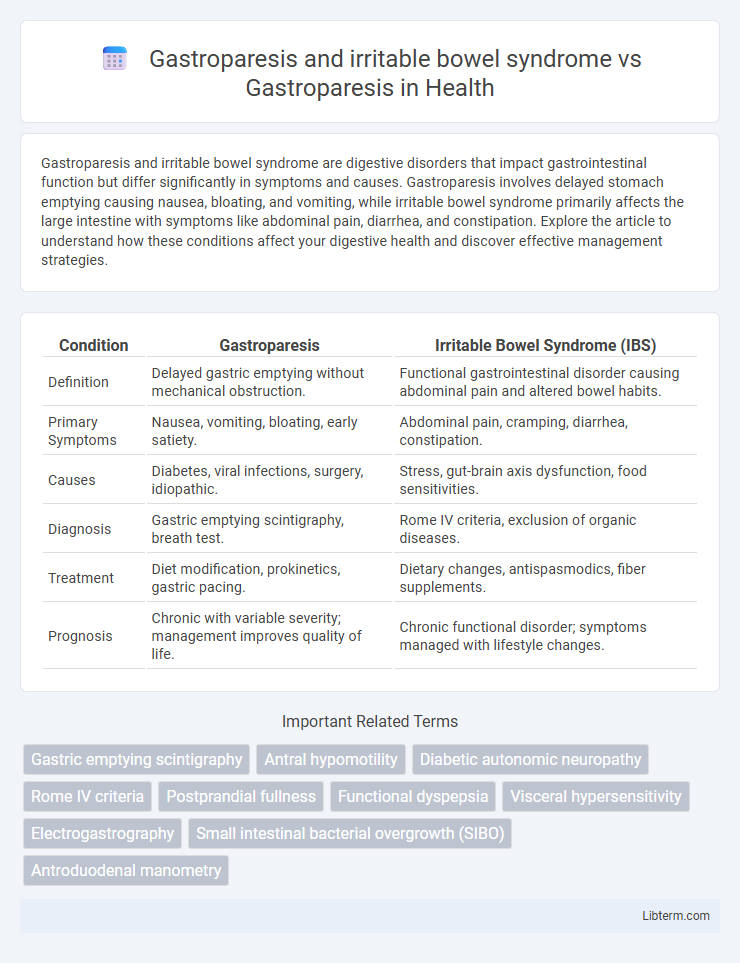
| Condition | Gastroparesis | Irritable Bowel Syndrome (IBS) |
|---|---|---|
| Definition | Delayed gastric emptying without mechanical obstruction. | Functional gastrointestinal disorder causing abdominal pain and altered bowel habits. |
| Primary Symptoms | Nausea, vomiting, bloating, early satiety. | Abdominal pain, cramping, diarrhea, constipation. |
| Causes | Diabetes, viral infections, surgery, idiopathic. | Stress, gut-brain axis dysfunction, food sensitivities. |
| Diagnosis | Gastric emptying scintigraphy, breath test. | Rome IV criteria, exclusion of organic diseases. |
| Treatment | Diet modification, prokinetics, gastric pacing. | Dietary changes, antispasmodics, fiber supplements. |
| Prognosis | Chronic with variable severity; management improves quality of life. | Chronic functional disorder; symptoms managed with lifestyle changes. |
Understanding Gastroparesis: Causes, Symptoms, and Diagnosis
Gastroparesis is a chronic condition characterized by delayed stomach emptying due to impaired gastric motility, often caused by diabetes, surgery, or neurological disorders. Symptoms include nausea, vomiting, early satiety, and abdominal pain, which can overlap with irritable bowel syndrome (IBS) but differ in underlying pathophysiology and diagnostic criteria. Diagnosis involves gastric emptying studies, upper endoscopy, and ruling out other gastrointestinal disorders like IBS that primarily affect bowel function rather than gastric motility.
What is Irritable Bowel Syndrome (IBS)? Key Facts Explained
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits such as diarrhea, constipation, or both. Unlike gastroparesis, which involves delayed stomach emptying due to impaired gastric motility, IBS primarily affects the large intestine and involves abnormal muscle contractions and heightened gut sensitivity. Understanding the distinct pathophysiology of IBS versus gastroparesis is crucial for accurate diagnosis and targeted treatment approaches in managing these digestive disorders.
Gastroparesis vs. IBS: Key Similarities and Differences
Gastroparesis and irritable bowel syndrome (IBS) both involve gastrointestinal dysfunction but differ significantly in pathophysiology and symptom presentation. Gastroparesis is characterized by delayed gastric emptying due to impaired stomach motility, often leading to nausea, vomiting, and bloating, whereas IBS primarily involves abnormal bowel motility and sensitivity causing abdominal pain, diarrhea, or constipation without structural abnormalities. Diagnostic approaches vary, with gastric emptying studies essential for Gastroparesis, while IBS diagnosis relies on symptom-based Rome IV criteria and exclusion of organic diseases.
Overlapping Symptoms: Navigating Digestive Disorders
Gastroparesis and irritable bowel syndrome (IBS) share overlapping symptoms such as abdominal pain, bloating, nausea, and altered bowel habits, complicating diagnosis and treatment. Both disorders affect gastrointestinal motility but differ in underlying mechanisms: gastroparesis involves delayed gastric emptying due to nerve dysfunction, while IBS is characterized by a brain-gut interaction causing visceral hypersensitivity and motility irregularities. Differentiating these conditions requires comprehensive diagnostic testing, including gastric emptying studies for gastroparesis and symptom-based criteria for IBS, to tailor effective management strategies.
Diagnosing Gastroparesis: Tests and Evaluation
Diagnosing gastroparesis involves specialized tests such as gastric emptying scintigraphy, which measures the rate at which food leaves the stomach, distinguishing it from irritable bowel syndrome (IBS) whose symptoms overlap but primarily involve colon motility. Other diagnostic tools include the breath test for assessing gastric emptying and upper endoscopy to exclude mechanical obstructions. Accurate evaluation of gastroparesis relies on symptom assessment combined with objective measurement of gastric motility, contrasting the functional bowel disruptions seen in IBS.
Diagnostic Approach: IBS versus Gastroparesis
The diagnostic approach to irritable bowel syndrome (IBS) primarily relies on symptom-based criteria such as the Rome IV guidelines, with emphasis on abdominal pain and altered bowel habits, while excluding organic diseases through basic laboratory tests and colonoscopy if needed. Gastroparesis diagnosis involves objective gastric emptying studies, such as scintigraphy or breath tests, to confirm delayed gastric motility, differentiating it from functional disorders like IBS. Unlike IBS, gastroparesis requires detailed evaluation of gastric motor function for accurate diagnosis and tailored management.
Treatment Options for Gastroparesis
Treatment options for gastroparesis focus on improving gastric motility and managing symptoms using prokinetic agents such as metoclopramide and erythromycin, dietary modifications like small, frequent low-fat meals, and in severe cases, gastric electrical stimulation or surgical interventions. Unlike irritable bowel syndrome (IBS), which is primarily managed through dietary changes, stress management, and antispasmodics, gastroparesis requires targeted therapies to address delayed gastric emptying. Optimizing glucose control in diabetic gastroparesis patients also plays a crucial role in symptom management and treatment efficacy.
Managing IBS: Dietary and Lifestyle Strategies
Managing IBS with dietary strategies involves increasing soluble fiber intake, avoiding trigger foods like caffeine and high-FODMAP items, and maintaining regular meal patterns to reduce symptoms. Incorporating stress reduction techniques and regular physical activity supports gastrointestinal motility and overall gut health in IBS patients. These lifestyle adjustments differ from gastroparesis management, which emphasizes small, low-fat meals and often requires medical interventions to address delayed gastric emptying.
Living with Gastroparesis and IBS: Coping Mechanisms
Living with gastroparesis and irritable bowel syndrome (IBS) necessitates tailored dietary adjustments such as low-fat, low-fiber meals to ease gastric emptying and bowel symptoms. Incorporating stress management techniques like mindfulness and cognitive behavioral therapy (CBT) helps alleviate symptom severity and improve quality of life. Regular consultation with gastroenterologists and nutritionists ensures personalized treatment plans that address both delayed gastric emptying and IBS-related motility issues effectively.
Gastroparesis vs. Combined Gastroparesis-IBS: Patient Outcomes
Gastroparesis causes delayed gastric emptying leading to symptoms like nausea and bloating, while combined gastroparesis-IBS presents with both gastric motility issues and altered bowel habits, complicating diagnosis and treatment. Patients with combined gastroparesis-IBS often experience more severe gastrointestinal discomfort, impaired quality of life, and higher healthcare utilization compared to those with gastroparesis alone. Effective management requires a multidisciplinary approach targeting gastric emptying improvement and IBS symptom control to optimize patient outcomes.
Gastroparesis and irritable bowel syndrome Infographic
 libterm.com
libterm.com