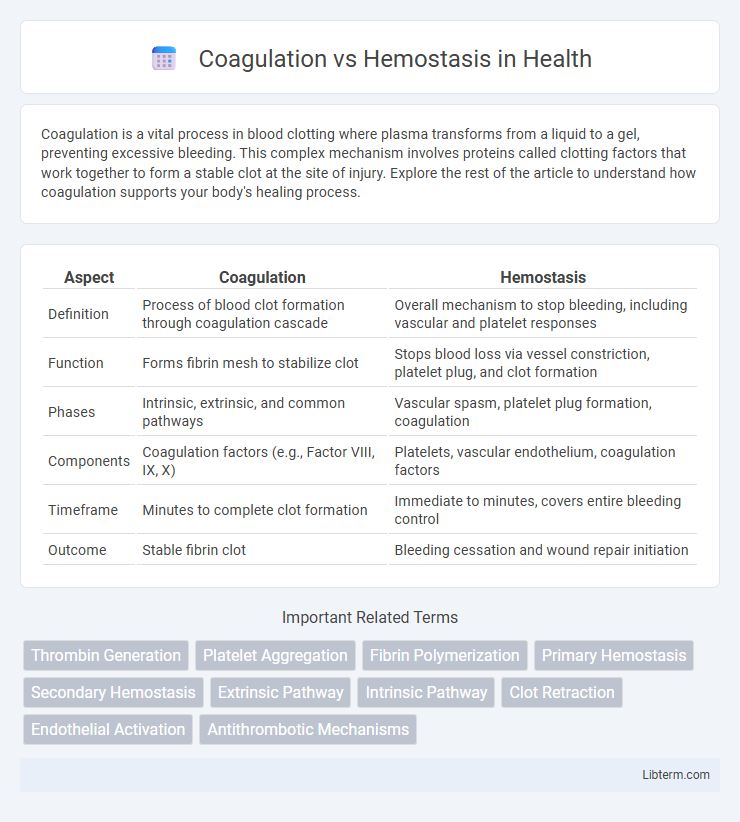
Coagulation is a vital process in blood clotting where plasma transforms from a liquid to a gel, preventing excessive bleeding. This complex mechanism involves proteins called clotting factors that work together to form a stable clot at the site of injury. Explore the rest of the article to understand how coagulation supports your body's healing process.
Table of Comparison
| Aspect | Coagulation | Hemostasis |
|---|---|---|
| Definition | Process of blood clot formation through coagulation cascade | Overall mechanism to stop bleeding, including vascular and platelet responses |
| Function | Forms fibrin mesh to stabilize clot | Stops blood loss via vessel constriction, platelet plug, and clot formation |
| Phases | Intrinsic, extrinsic, and common pathways | Vascular spasm, platelet plug formation, coagulation |
| Components | Coagulation factors (e.g., Factor VIII, IX, X) | Platelets, vascular endothelium, coagulation factors |
| Timeframe | Minutes to complete clot formation | Immediate to minutes, covers entire bleeding control |
| Outcome | Stable fibrin clot | Bleeding cessation and wound repair initiation |
Introduction to Coagulation and Hemostasis
Coagulation and hemostasis are critical physiological processes that prevent excessive bleeding by forming blood clots at injury sites. Hemostasis involves vascular constriction, platelet aggregation, and the coagulation cascade, which stabilizes the platelet plug through fibrin mesh formation. The coagulation cascade activates a series of clotting factors, leading to thrombin generation and fibrin clot development essential for wound repair.
Defining Coagulation: Key Processes
Coagulation is a complex biological process essential for stopping bleeding by transforming blood from a liquid to a gel, forming a stable fibrin clot. Key processes include the activation of clotting factors through intrinsic and extrinsic pathways, leading to the conversion of prothrombin to thrombin, which then converts fibrinogen into fibrin strands. This cascade is tightly regulated to prevent excessive clotting and maintain vascular integrity during hemostasis.
Understanding Hemostasis: Stages and Functions
Hemostasis involves a complex physiological process with three key stages: vascular spasm, platelet plug formation, and coagulation, each essential for preventing excessive blood loss. During vascular spasm, injured blood vessels constrict to reduce blood flow, while platelet aggregation forms a temporary plug at the injury site. Coagulation solidifies the platelet plug by generating a fibrin mesh through the activation of clotting factors in intrinsic and extrinsic pathways, stabilizing the wound and initiating tissue repair.
Major Differences Between Coagulation and Hemostasis
Coagulation is a complex biochemical process involving a cascade of clotting factors that leads to the formation of a fibrin clot, while hemostasis is a broader physiological response encompassing vascular spasm, platelet plug formation, and coagulation to prevent blood loss. Hemostasis includes primary hemostasis (platelet adhesion and aggregation) and secondary hemostasis (coagulation cascade leading to fibrin stabilization). Unlike coagulation, hemostasis involves both cellular and molecular mechanisms working together to achieve blood vessel repair and bleeding cessation.
The Coagulation Cascade: Steps and Factors
The coagulation cascade involves a sequence of enzymatic reactions essential for blood clot formation, primarily divided into the intrinsic, extrinsic, and common pathways. Key factors include Factor XII initiating the intrinsic pathway, Factor VII activating the extrinsic pathway, and Factors X, V, II (prothrombin), and I (fibrinogen) driving the common pathway to form a stable fibrin clot. Each step amplifies the response, culminating in the conversion of fibrinogen to fibrin by thrombin, solidifying the clot during hemostasis.
Role of Platelets in Hemostasis
Platelets play a critical role in hemostasis by adhering to the damaged vascular endothelium and forming a primary platelet plug to prevent blood loss. They release granules containing ADP, thromboxane A2, and other factors that promote platelet aggregation and vasoconstriction, essential steps in stabilizing the clot. Unlike coagulation, which involves a complex cascade of plasma proteins leading to fibrin clot formation, platelet activity is the initial response that rapidly controls bleeding.
Physiological Importance of Hemostasis
Hemostasis is a vital physiological process that prevents excessive blood loss following vascular injury by forming a stable blood clot, ensuring tissue integrity and survival. It involves vessel constriction, platelet aggregation, and a complex cascade of coagulation factors to quickly seal damaged vessels. This tightly regulated mechanism balances clot formation and dissolution to maintain normal blood flow and prevent hemorrhage or thrombosis.
Disorders Related to Coagulation and Hemostasis
Disorders related to coagulation and hemostasis include hemophilia, characterized by deficient clotting factors leading to excessive bleeding, and thrombophilia, which involves hyperactive clotting increasing the risk of thrombosis. Von Willebrand disease affects platelet adhesion and is the most common inherited bleeding disorder, while disseminated intravascular coagulation (DIC) causes widespread clotting and bleeding simultaneously, often complicating systemic infections or trauma. Effective diagnosis and management require understanding the intricate balance between coagulation factors, platelets, and fibrinolytic pathways to prevent hemorrhage or pathological thrombosis.
Diagnostic Evaluation of Coagulation vs. Hemostasis
Diagnostic evaluation of coagulation involves laboratory tests such as prothrombin time (PT), activated partial thromboplastin time (aPTT), thrombin time (TT), and fibrinogen assays to assess the clotting cascade and the function of coagulation factors. Hemostasis evaluation encompasses platelet count, bleeding time, and platelet function assays to analyze primary hemostasis and vascular integrity. Differentiating between coagulation and hemostasis disorders relies on combined testing strategies including viscoelastic tests like thromboelastography (TEG) or rotational thromboelastometry (ROTEM) to provide a comprehensive picture of clot formation and stability.
Therapeutic Approaches: Managing Coagulation and Hemostasis Issues
Therapeutic approaches for managing coagulation and hemostasis focus on precisely balancing clot formation and dissolution to prevent bleeding or thrombosis. Anticoagulants like warfarin and direct oral anticoagulants (DOACs) target specific coagulation factors to inhibit clot propagation, while hemostatic agents such as tranexamic acid and recombinant factor concentrates promote clot stabilization in bleeding disorders. Personalized treatment strategies involve monitoring coagulation profiles through assays like PT, aPTT, and thromboelastography to optimize dosing and reduce adverse events.
Coagulation Infographic
 libterm.com
libterm.com