Sarcopenia is the progressive loss of muscle mass and strength, significantly contributing to frailty in older adults, which increases vulnerability to falls, disability, and decreased quality of life. Early intervention through resistance training and proper nutrition can slow muscle deterioration and enhance physical resilience. Discover effective strategies to combat sarcopenia and manage frailty in the detailed article ahead.
Table of Comparison
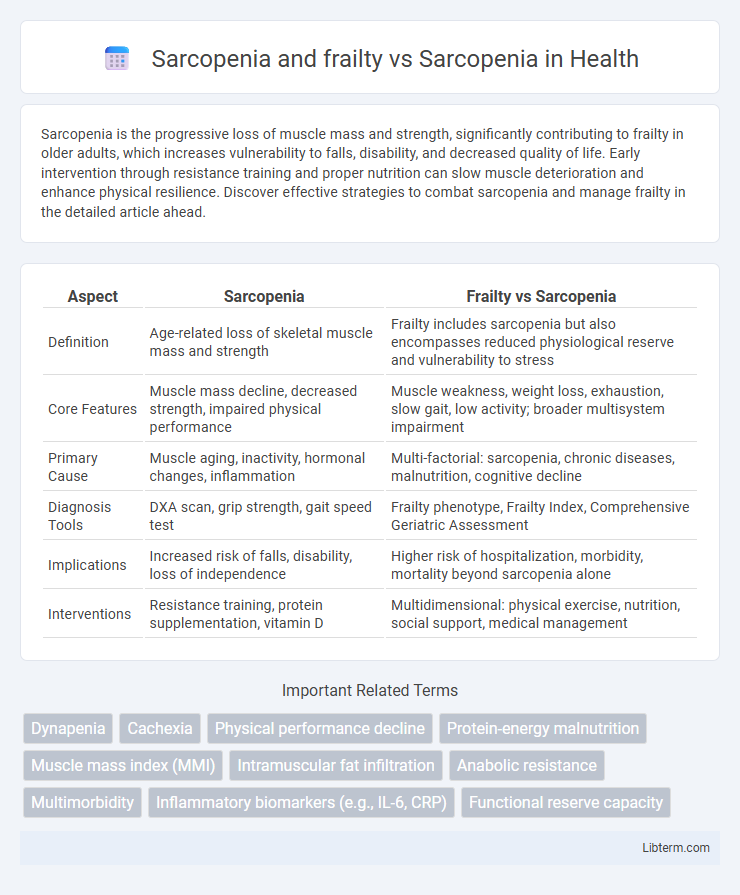
| Aspect | Sarcopenia | Frailty vs Sarcopenia |
|---|---|---|
| Definition | Age-related loss of skeletal muscle mass and strength | Frailty includes sarcopenia but also encompasses reduced physiological reserve and vulnerability to stress |
| Core Features | Muscle mass decline, decreased strength, impaired physical performance | Muscle weakness, weight loss, exhaustion, slow gait, low activity; broader multisystem impairment |
| Primary Cause | Muscle aging, inactivity, hormonal changes, inflammation | Multi-factorial: sarcopenia, chronic diseases, malnutrition, cognitive decline |
| Diagnosis Tools | DXA scan, grip strength, gait speed test | Frailty phenotype, Frailty Index, Comprehensive Geriatric Assessment |
| Implications | Increased risk of falls, disability, loss of independence | Higher risk of hospitalization, morbidity, mortality beyond sarcopenia alone |
| Interventions | Resistance training, protein supplementation, vitamin D | Multidimensional: physical exercise, nutrition, social support, medical management |
Understanding Sarcopenia: Definition and Key Features
Sarcopenia is a progressive loss of skeletal muscle mass and strength associated with aging, leading to decreased physical performance and increased risk of adverse outcomes. Frailty encompasses sarcopenia but also includes additional factors such as weight loss, exhaustion, and reduced endurance, reflecting a broader vulnerability to stressors. Understanding sarcopenia involves recognizing its key features like muscle atrophy, weakness, and impaired mobility, which are critical for early diagnosis and intervention.
Frailty Explained: Characteristics and Clinical Impact
Frailty is a multidimensional syndrome characterized by decreased strength, endurance, and physiological function, increasing vulnerability to adverse health outcomes, often overlapping with but distinct from sarcopenia, which specifically involves the loss of muscle mass and function. Clinical impact of frailty includes higher risks of falls, hospitalization, disability, and mortality, necessitating early identification and comprehensive management to improve patient outcomes. Assessments using tools like the Fried Frailty Criteria or Rockwood Frailty Index help differentiate frailty from sarcopenia, guiding targeted interventions.
Sarcopenia vs Frailty: Key Differences and Overlaps
Sarcopenia is defined by the progressive loss of muscle mass and strength, primarily impacting physical performance, whereas frailty encompasses a broader syndrome including weight loss, exhaustion, low physical activity, and slow walking speed alongside muscle deterioration. Both conditions increase the risk of adverse outcomes such as falls, disability, and mortality, but frailty reflects a multidimensional state of vulnerability beyond muscle impairment alone. Identifying and addressing the overlap between sarcopenia and frailty enables targeted interventions to improve the health and functional independence of older adults.
Epidemiology: Prevalence in Aging Populations
Sarcopenia affects approximately 10-40% of adults over 60, with prevalence increasing sharply after age 70. Frailty, often overlapping with sarcopenia, occurs in about 7-16% of older adults, rising to 25-50% in those over 85. Epidemiological studies reveal that sarcopenia alone predicts muscle mass loss, while frailty encompasses broader vulnerability, including declines in strength, endurance, and physiological function.
Pathophysiological Mechanisms: Sarcopenia Alone vs Combined with Frailty
Sarcopenia involves progressive loss of skeletal muscle mass and strength driven by mitochondrial dysfunction, inflammatory cytokines, and hormonal changes such as decreased IGF-1 and testosterone. When combined with frailty, pathophysiological mechanisms intensify, incorporating multi-system dysregulation including impaired energy metabolism, neuronal degeneration, and chronic systemic inflammation, exacerbating vulnerability to stressors. The interaction between sarcopenia and frailty accelerates muscle degradation and functional decline through altered protein synthesis, increased oxidative stress, and compromised neuromuscular junction integrity.
Diagnostic Criteria: Assessment Tools for Sarcopenia and Frailty
Diagnostic criteria for sarcopenia primarily rely on assessing muscle mass, strength, and physical performance using tools such as dual-energy X-ray absorptiometry (DXA), handgrip dynamometry, and gait speed measurement. Frailty assessment expands beyond muscle evaluation to include multidimensional tools like the Fried Frailty Phenotype and the Frailty Index, which incorporate criteria such as weight loss, exhaustion, and activity levels alongside sarcopenia markers. Accurate differentiation between sarcopenia and frailty through these targeted assessment tools is critical for tailored intervention planning in elderly populations.
Functional Consequences: Health Outcomes and Risks
Sarcopenia significantly contributes to frailty, exacerbating risks of falls, disability, and mortality in older adults due to impaired muscle strength and physical performance. Frailty, characterized by decreased physiological reserves, compounds the functional decline seen in sarcopenia, leading to higher vulnerability to adverse health outcomes such as hospitalization and prolonged recovery. Addressing sarcopenia alone improves muscle function, but tackling frailty involves comprehensive interventions targeting multiple physiological systems to reduce cumulative health risks.
Management Strategies: Targeted Interventions for Sarcopenia and Frailty
Management strategies for sarcopenia and frailty emphasize targeted interventions such as resistance training, nutritional supplementation, and comprehensive geriatric assessment to improve muscle strength and functional performance. Resistance exercise protocols combined with protein-rich diets and vitamin D supplementation have demonstrated efficacy in mitigating muscle loss and physical decline in older adults. Multidisciplinary approaches integrating physical therapy, pharmacological treatments, and psychosocial support optimize outcomes for individuals with sarcopenia and frailty.
Preventative Approaches: Lifestyle and Nutritional Considerations
Preventative approaches for sarcopenia and frailty emphasize resistance training and protein-rich diets to maintain muscle mass and function. Incorporating vitamin D supplementation and omega-3 fatty acids supports muscle strength and reduces inflammation, crucial for older adults at risk. Regular physical activity combined with adequate nutrient intake optimizes musculoskeletal health, reducing the incidence of both sarcopenia and frailty.
Future Directions: Research and Clinical Implications
Future research on sarcopenia and frailty emphasizes developing precise biomarkers and advanced imaging techniques for early detection and differentiation between these conditions. Clinical implications include tailored interventions combining resistance training, nutritional supplementation, and pharmacological therapies to improve muscle function and reduce adverse outcomes in aging populations. Innovative approaches integrating digital health tools aim to enhance patient monitoring and optimize individualized treatment strategies.
Sarcopenia and frailty Infographic
 libterm.com
libterm.com