Neoadjuvant therapy refers to treatments given before the main treatment, often surgery, to shrink tumors and improve outcomes. This approach can increase the chances of successful tumor removal and reduce the risk of recurrence. Discover how neoadjuvant therapy can impact your treatment plan by reading the full article.
Table of Comparison
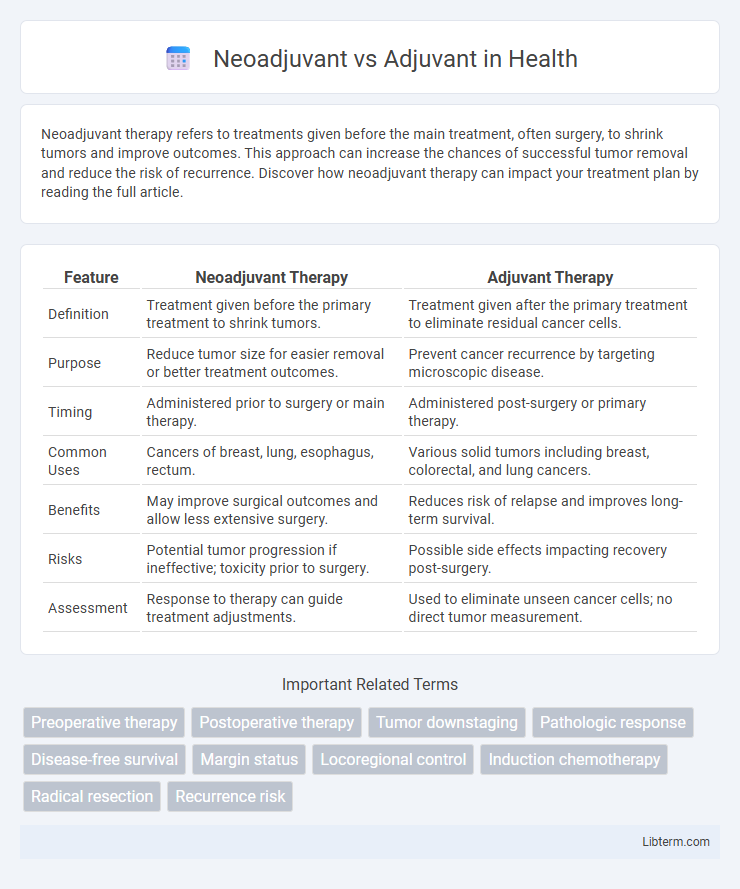
| Feature | Neoadjuvant Therapy | Adjuvant Therapy |
|---|---|---|
| Definition | Treatment given before the primary treatment to shrink tumors. | Treatment given after the primary treatment to eliminate residual cancer cells. |
| Purpose | Reduce tumor size for easier removal or better treatment outcomes. | Prevent cancer recurrence by targeting microscopic disease. |
| Timing | Administered prior to surgery or main therapy. | Administered post-surgery or primary therapy. |
| Common Uses | Cancers of breast, lung, esophagus, rectum. | Various solid tumors including breast, colorectal, and lung cancers. |
| Benefits | May improve surgical outcomes and allow less extensive surgery. | Reduces risk of relapse and improves long-term survival. |
| Risks | Potential tumor progression if ineffective; toxicity prior to surgery. | Possible side effects impacting recovery post-surgery. |
| Assessment | Response to therapy can guide treatment adjustments. | Used to eliminate unseen cancer cells; no direct tumor measurement. |
Introduction to Neoadjuvant and Adjuvant Therapies
Neoadjuvant therapies refer to treatments given before the primary intervention, typically surgery, to reduce tumor size and improve surgical outcomes in cancer management. Adjuvant therapies are administered after the main treatment to eliminate residual disease and decrease the risk of cancer recurrence. Both approaches play critical roles in multimodal cancer treatment protocols to enhance patient survival rates.
Defining Neoadjuvant Therapy
Neoadjuvant therapy refers to treatments such as chemotherapy, radiation, or hormone therapy administered before the primary surgical intervention to shrink tumors and improve resectability. This therapeutic approach aims to reduce tumor size, eradicate micrometastases, and enhance surgical outcomes, particularly in cancers like breast, lung, and esophageal tumors. Neoadjuvant therapy differs from adjuvant therapy, which is given post-surgery to eliminate residual cancer cells and lower recurrence risk.
Understanding Adjuvant Therapy
Adjuvant therapy involves treatments given after primary surgery to eliminate remaining cancer cells and reduce the risk of recurrence, commonly including chemotherapy, radiation, or hormone therapy. This approach targets microscopic disease that surgery might miss, improving long-term survival rates in cancers like breast, colorectal, and lung cancer. Understanding the timing and purpose of adjuvant therapy is essential for optimizing patient outcomes and tailoring personalized cancer treatment plans.
Key Differences Between Neoadjuvant and Adjuvant Treatments
Neoadjuvant treatments are administered before the primary therapy, typically surgery, to shrink tumors and improve surgical outcomes, whereas adjuvant treatments are given after surgery to eliminate residual cancer cells and reduce recurrence risk. Neoadjuvant therapy allows for early assessment of tumor response and may enable less extensive surgery, while adjuvant therapy targets microscopic disease remaining postoperatively. The choice between neoadjuvant and adjuvant treatments depends on tumor type, stage, and patient factors, with breast and rectal cancers frequently utilizing both approaches based on clinical protocols.
Indications for Neoadjuvant Versus Adjuvant Approaches
Neoadjuvant therapy is primarily indicated for patients with locally advanced tumors where tumor size reduction can facilitate surgical resection or improve the likelihood of breast-conserving surgery, particularly in breast, esophageal, and rectal cancers. Adjuvant therapy is typically recommended post-surgery to eliminate residual microscopic disease and reduce recurrence risk, especially in early-stage cancers with high-risk pathological features such as lymph node involvement or positive margins. The choice between neoadjuvant and adjuvant approaches depends on tumor staging, biological markers, and the potential to improve surgical outcomes or long-term survival.
Clinical Benefits of Neoadjuvant Therapy
Neoadjuvant therapy offers significant clinical benefits by reducing tumor size before surgery, which can enhance surgical outcomes and increase the likelihood of breast-conserving procedures. This approach enables early assessment of tumor response to treatment, providing valuable prognostic information and guiding subsequent therapeutic decisions. Evidence from clinical studies shows that neoadjuvant therapy can improve overall survival rates and decrease the risk of micrometastatic spread compared to adjuvant therapy administered postoperatively.
Advantages of Adjuvant Therapy
Adjuvant therapy enhances the effectiveness of primary treatments by targeting residual cancer cells post-surgery, reducing recurrence rates and improving overall survival. This therapy allows for precise pathological assessment before treatment, enabling tailored systemic treatments based on tumor characteristics. It also supports better patient recovery by postponing systemic therapy until after surgical wound healing, minimizing treatment-related complications.
Factors Influencing Treatment Choice
Factors influencing the choice between neoadjuvant and adjuvant therapy include tumor size, stage, and patient overall health. Molecular and genetic tumor profiles often guide the decision toward neoadjuvant treatment to shrink tumors before surgery. Patient response to chemotherapy, risk of metastasis, and potential surgical outcomes critically determine the timing and type of adjuvant therapy administered.
Current Research and Emerging Trends
Current research in oncology highlights significant advances in neoadjuvant therapies, particularly with immunotherapy and targeted agents showing promise in shrinking tumors pre-surgery to improve resectability and survival outcomes. Emerging trends emphasize personalized medicine approaches, leveraging genomic profiling to tailor neoadjuvant and adjuvant treatments, optimizing efficacy while minimizing toxicity. Studies increasingly compare long-term survival and recurrence rates between neoadjuvant and adjuvant modalities, refining clinical guidelines for cancers such as breast, lung, and colorectal cancers.
Conclusion: Optimizing Patient Outcomes
Neoadjuvant therapy, administered before surgery, can reduce tumor size and improve surgical outcomes, while adjuvant therapy targets residual cancer cells post-surgery to minimize recurrence risk. Personalized treatment plans integrating molecular profiling and tumor characteristics optimize the timing and selection of therapies, enhancing overall survival rates and quality of life. Multidisciplinary coordination ensures the most effective approach, balancing efficacy and toxicity to achieve optimal patient outcomes.
Neoadjuvant Infographic
 libterm.com
libterm.com