Lymphocytosis is a condition characterized by an elevated number of lymphocytes in the blood, often indicating an immune response to infections, chronic inflammation, or certain hematologic diseases. Understanding the causes and implications of lymphocytosis can help in diagnosing underlying health issues and determining appropriate treatment strategies. Discover more about the symptoms, causes, and management of lymphocytosis in the rest of the article.
Table of Comparison
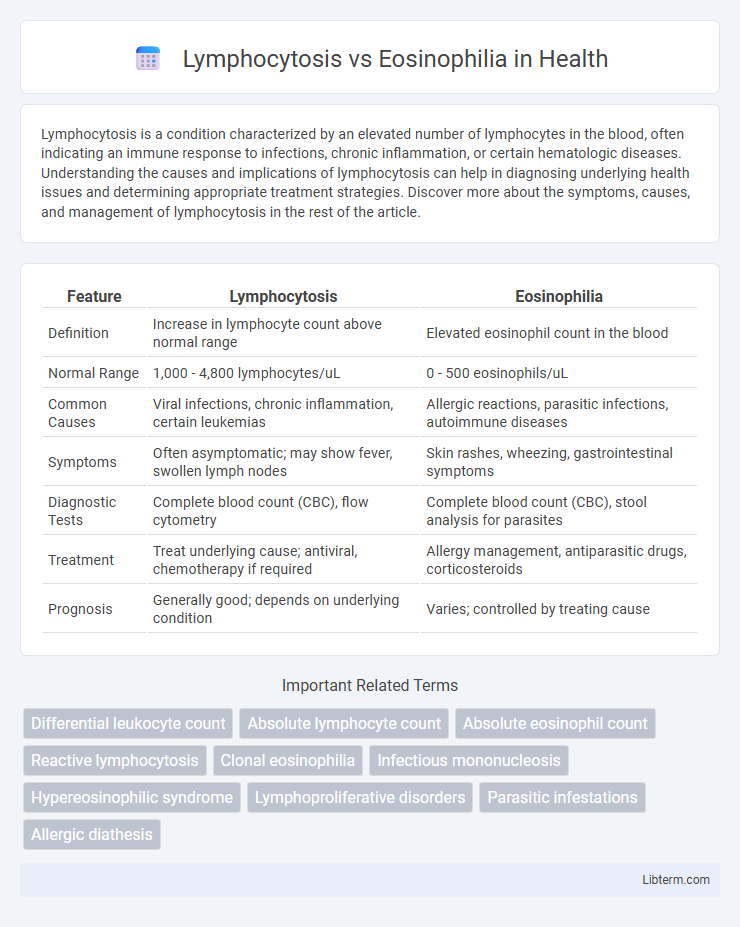
| Feature | Lymphocytosis | Eosinophilia |
|---|---|---|
| Definition | Increase in lymphocyte count above normal range | Elevated eosinophil count in the blood |
| Normal Range | 1,000 - 4,800 lymphocytes/uL | 0 - 500 eosinophils/uL |
| Common Causes | Viral infections, chronic inflammation, certain leukemias | Allergic reactions, parasitic infections, autoimmune diseases |
| Symptoms | Often asymptomatic; may show fever, swollen lymph nodes | Skin rashes, wheezing, gastrointestinal symptoms |
| Diagnostic Tests | Complete blood count (CBC), flow cytometry | Complete blood count (CBC), stool analysis for parasites |
| Treatment | Treat underlying cause; antiviral, chemotherapy if required | Allergy management, antiparasitic drugs, corticosteroids |
| Prognosis | Generally good; depends on underlying condition | Varies; controlled by treating cause |
Understanding Lymphocytosis: Definition and Causes
Lymphocytosis is characterized by an elevated lymphocyte count in the blood, typically exceeding 4,000 lymphocytes per microliter in adults, often signaling viral infections such as infectious mononucleosis or chronic lymphocytic leukemia. This condition differs from eosinophilia, which involves increased eosinophils linked to allergic reactions, parasitic infections, or certain autoimmune disorders. Recognizing the distinct cellular profiles and underlying causes is crucial for accurate diagnosis and targeted treatment strategies.
Eosinophilia Explained: Overview and Triggers
Eosinophilia is characterized by an elevated eosinophil count in the blood, often exceeding 500 cells per microliter, and is primarily triggered by allergic reactions, parasitic infections, autoimmune diseases, and certain malignancies. This condition involves the proliferation and activation of eosinophils, a type of white blood cell integral to immune response and inflammation regulation. Distinct from lymphocytosis, which involves increased lymphocytes due to viral infections or certain cancers, eosinophilia's key markers include heightened eosinophil-related cytokines such as interleukin-5 (IL-5) and associated tissue damage caused by eosinophil degranulation.
Key Differences Between Lymphocytosis and Eosinophilia
Lymphocytosis is characterized by an elevated lymphocyte count, often associated with viral infections, chronic inflammatory conditions, or certain lymphoproliferative disorders, whereas eosinophilia involves an increased eosinophil count commonly linked to allergic reactions, parasitic infections, and some autoimmune diseases. The key diagnostic difference lies in the specific white blood cell type elevated, with lymphocytes primarily responsible for adaptive immunity and eosinophils playing a central role in combating parasitic infections and mediating allergic responses. Clinical implications vary as lymphocytosis may indicate viral or hematologic disorders, while eosinophilia typically suggests allergic or parasitic etiologies requiring different treatment approaches.
Clinical Manifestations of Lymphocytosis
Lymphocytosis presents clinically with persistent lymphadenopathy, splenomegaly, and symptoms of viral infections such as fatigue, fever, and night sweats. Patients may also exhibit signs of chronic lymphocytic leukemia including easy bruising and recurrent infections due to compromised immune function. Physical examination often reveals enlarged lymph nodes and hepatosplenomegaly, distinguishing it from eosinophilia, which primarily involves allergic reactions and parasitic infections.
Common Symptoms Associated with Eosinophilia
Eosinophilia is characterized by an elevated eosinophil count in the blood, commonly presenting symptoms such as skin rashes, itching, and respiratory issues like wheezing or cough due to allergic reactions or parasitic infections. Unlike lymphocytosis, which involves increased lymphocytes often seen with viral infections and may cause fever and swollen lymph nodes, eosinophilia symptoms are more related to hypersensitivity responses and tissue inflammation. Persistent eosinophilia can also lead to organ damage, particularly in the lungs, heart, and gastrointestinal tract, necessitating targeted diagnostic evaluation.
Diagnostic Approaches for Lymphocytosis vs Eosinophilia
Diagnostic approaches for lymphocytosis prioritize complete blood count (CBC) with differential to quantify lymphocyte levels, alongside flow cytometry for immunophenotyping to distinguish reactive from clonal lymphocyte expansions. In contrast, eosinophilia diagnosis emphasizes CBC with differential to identify eosinophil counts, while bone marrow biopsy and serum IgE levels help determine underlying causes such as allergic reactions or hematologic malignancies. Molecular tests and parasitic infection screening refine diagnosis for both conditions by targeting specific etiologies contributing to abnormal lymphocyte or eosinophil proliferation.
Underlying Diseases Linked to Each Condition
Lymphocytosis is commonly associated with viral infections such as infectious mononucleosis, chronic lymphocytic leukemia, and certain autoimmune disorders like rheumatoid arthritis, reflecting an immune response involving increased lymphocyte production. Eosinophilia often indicates allergic diseases including asthma and atopic dermatitis, parasitic infections like helminthiasis, and some malignancies such as Hodgkin lymphoma, characterized by elevated eosinophil counts in peripheral blood. Differentiating these conditions is critical for accurate diagnosis and treatment, as their underlying diseases reflect distinct immunological pathways and clinical implications.
Treatment Options for Lymphocytosis and Eosinophilia
Treatment options for lymphocytosis often target underlying infections or chronic conditions, using antiviral or antibacterial medications, corticosteroids, or chemotherapy in cases of lymphoproliferative disorders. Eosinophilia treatment centers on identifying and eliminating allergenic triggers, parasitic infections, or autoimmune diseases, with corticosteroids, antihistamines, and immunosuppressive agents commonly prescribed. Both conditions may require hematologic evaluation to determine severity and guide appropriate therapy.
Prognosis and Complications
Lymphocytosis often indicates viral infections or chronic inflammatory conditions and generally has a favorable prognosis with mild complications unless associated with hematologic malignancies. Eosinophilia is linked to allergic reactions, parasitic infections, or autoimmune diseases, and its prognosis varies depending on the underlying cause, with potential complications including tissue damage and organ dysfunction. Persistent or severe eosinophilia can lead to complications such as eosinophilic myocarditis or pulmonary fibrosis, while lymphocytosis rarely causes direct organ damage.
When to Seek Medical Evaluation
Seek medical evaluation for lymphocytosis if you experience persistent symptoms like unexplained weight loss, night sweats, or swollen lymph nodes, as these may indicate infections, chronic inflammatory conditions, or blood cancers. Eosinophilia warrants prompt medical attention when accompanied by asthma exacerbations, allergic reactions, or signs of organ damage, suggesting underlying parasitic infections, allergic diseases, or autoimmune syndromes. Early diagnosis through blood tests and clinical assessment is crucial to determine the cause and guide appropriate treatment for both conditions.
Lymphocytosis Infographic
 libterm.com
libterm.com