Hypocalcemia is a condition characterized by low levels of calcium in the blood, which can lead to symptoms such as muscle cramps, tingling, and fatigue. It often results from vitamin D deficiency, kidney disease, or parathyroid gland disorders affecting calcium regulation. Discover more about hypocalcemia's causes, symptoms, and treatment options to manage your health effectively.
Table of Comparison
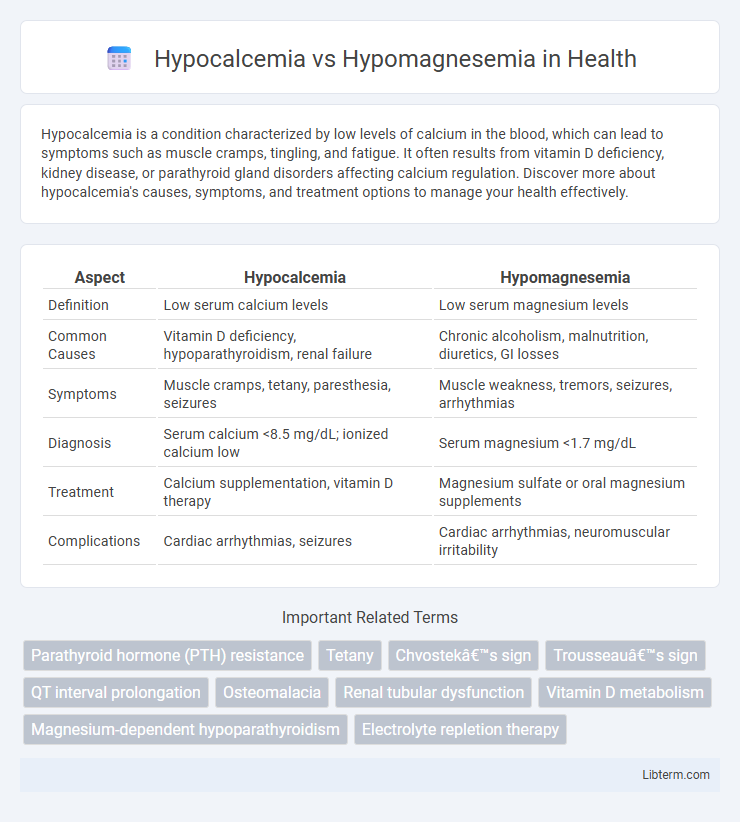
| Aspect | Hypocalcemia | Hypomagnesemia |
|---|---|---|
| Definition | Low serum calcium levels | Low serum magnesium levels |
| Common Causes | Vitamin D deficiency, hypoparathyroidism, renal failure | Chronic alcoholism, malnutrition, diuretics, GI losses |
| Symptoms | Muscle cramps, tetany, paresthesia, seizures | Muscle weakness, tremors, seizures, arrhythmias |
| Diagnosis | Serum calcium <8.5 mg/dL; ionized calcium low | Serum magnesium <1.7 mg/dL |
| Treatment | Calcium supplementation, vitamin D therapy | Magnesium sulfate or oral magnesium supplements |
| Complications | Cardiac arrhythmias, seizures | Cardiac arrhythmias, neuromuscular irritability |
Overview of Hypocalcemia and Hypomagnesemia
Hypocalcemia is characterized by low serum calcium levels, often causing muscle cramps, tetany, and cardiac arrhythmias due to impaired neuromuscular function. Hypomagnesemia involves reduced blood magnesium concentrations, leading to symptoms such as muscle weakness, tremors, and cardiac dysrhythmias as magnesium is crucial for cellular metabolism and neuromuscular stability. Both electrolyte imbalances can coexist, with hypomagnesemia frequently contributing to refractory hypocalcemia by impairing parathyroid hormone secretion and action.
Causes of Hypocalcemia
Hypocalcemia primarily results from vitamin D deficiency, hypoparathyroidism, and chronic kidney disease, which impair calcium absorption and regulation. Magnesium deficiency, while causing hypomagnesemia, also disrupts parathyroid hormone secretion, indirectly contributing to hypocalcemia. Other causes include acute pancreatitis and certain medications like bisphosphonates, which affect calcium metabolism.
Causes of Hypomagnesemia
Hypomagnesemia primarily results from gastrointestinal losses such as chronic diarrhea, malabsorption syndromes, or prolonged use of proton pump inhibitors, which impair magnesium absorption. Other significant causes include renal magnesium wasting due to diuretics, genetic disorders, or uncontrolled diabetes mellitus leading to increased magnesium excretion. Alcoholism often contributes to hypomagnesemia by causing poor dietary intake, increased renal clearance, and intracellular shifts of magnesium.
Pathophysiology: Calcium vs Magnesium Deficiency
Hypocalcemia results from decreased calcium levels, often due to parathyroid hormone deficiency or vitamin D abnormalities, impairing bone metabolism and neuromuscular function. Hypomagnesemia arises from insufficient magnesium, disrupting enzymatic reactions and altering calcium and potassium balance. Both deficiencies affect cellular ion transport but differ in underlying mechanisms and clinical manifestations.
Clinical Manifestations: Differentiating Symptoms
Hypocalcemia commonly presents with neuromuscular irritability such as tetany, muscle cramps, and positive Trousseau's or Chvostek's signs, while hypomagnesemia often manifests with muscle weakness, tremors, and seizures. Cardiac arrhythmias and prolonged QT interval can occur in both, but hypomagnesemia is more frequently associated with refractory hypokalemia due to renal potassium wasting. Differentiating these clinical symptoms aids in accurate diagnosis and targeted electrolyte correction.
Diagnostic Approaches
Diagnostic approaches for hypocalcemia primarily involve measuring serum total and ionized calcium levels, along with assessing parathyroid hormone (PTH) concentrations to distinguish between PTH-dependent and independent causes. In contrast, hypomagnesemia diagnosis requires serum magnesium measurement and evaluation of magnesium excretion in urine to determine renal wasting or gastrointestinal loss. Both conditions benefit from concurrent assessment of electrolytes such as potassium and phosphate, which can provide insight into underlying systemic disorders or coexisting deficiencies.
Laboratory Findings Comparison
Hypocalcemia presents with low serum calcium levels typically below 8.5 mg/dL, often accompanied by elevated parathyroid hormone (PTH) in cases of secondary hypocalcemia, while hypomagnesemia shows serum magnesium levels under 1.7 mg/dL and frequently causes secondary hypocalcemia due to impaired PTH secretion or action. Laboratory findings in hypocalcemia include low ionized calcium, normal or elevated phosphate, and possibly low vitamin D levels, whereas hypomagnesemia is characterized by concurrent hypokalemia and hypocalcemia with normal or low PTH. Diagnosing these conditions requires measuring serum electrolytes including calcium, magnesium, phosphate, PTH, and 25-hydroxyvitamin D to guide appropriate treatment strategies.
Treatment Strategies for Hypocalcemia
Treatment strategies for hypocalcemia primarily involve calcium supplementation through oral or intravenous routes, depending on severity, alongside vitamin D administration to enhance calcium absorption. Monitoring and addressing underlying causes such as hypoparathyroidism or magnesium deficiency is crucial, as correcting hypomagnesemia can improve calcium levels by restoring parathyroid hormone function. Regular serum calcium and magnesium level assessments guide therapy adjustments and prevent complications like tetany or cardiac arrhythmias.
Management of Hypomagnesemia
Management of hypomagnesemia involves magnesium supplementation through oral or intravenous routes depending on severity; mild cases typically receive oral magnesium oxide or magnesium gluconate, while severe symptomatic hypomagnesemia requires intravenous magnesium sulfate. Continuous monitoring of serum magnesium, calcium, and potassium levels is essential to prevent complications such as cardiac arrhythmias and neuromuscular irritability. Correction of underlying causes, including addressing malabsorption, chronic alcoholism, or medication effects like diuretics or proton pump inhibitors, is critical for effective long-term management.
Prognosis and Prevention
Hypocalcemia prognosis varies depending on the underlying cause, with chronic cases potentially leading to neuromuscular complications if untreated, whereas hypomagnesemia carries risks of cardiac arrhythmias and neurological symptoms that can improve with timely magnesium supplementation. Preventive measures for hypocalcemia include maintaining adequate dietary calcium and vitamin D intake, while hypomagnesemia prevention focuses on correcting magnesium deficiency through balanced nutrition and avoiding factors like chronic alcoholism or certain medications that impair magnesium absorption. Early diagnosis and management of electrolyte imbalances significantly enhance patient outcomes in both conditions.
Hypocalcemia Infographic
 libterm.com
libterm.com