Infectious diseases spread rapidly through populations, posing significant health risks worldwide. Understanding transmission methods and prevention strategies is crucial for protecting Your health and preventing outbreaks. Explore the rest of the article to learn how to stay safe and minimize infection risks effectively.
Table of Comparison
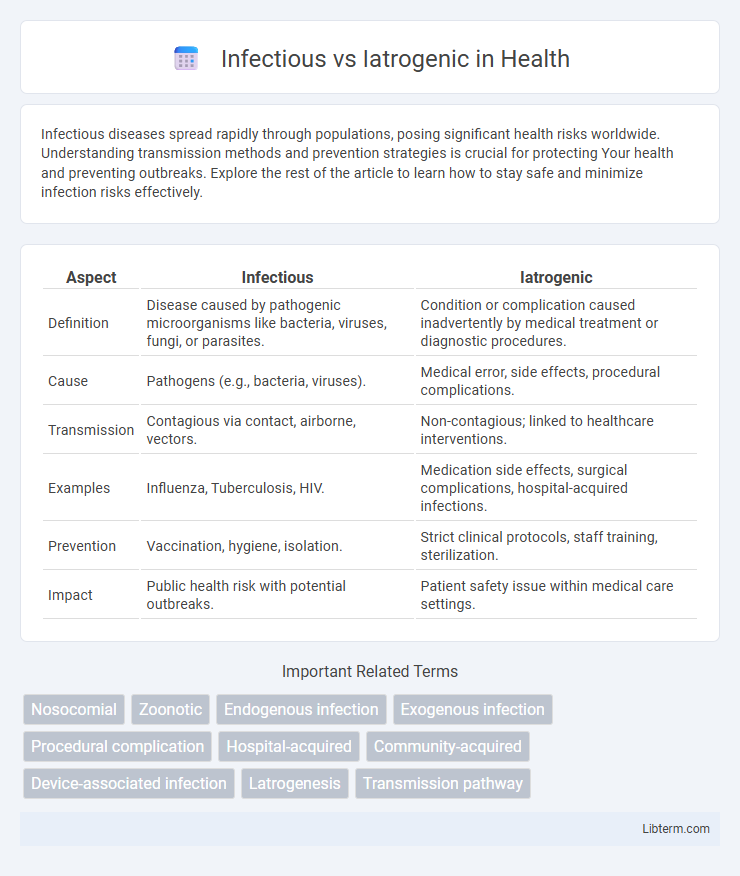
| Aspect | Infectious | Iatrogenic |
|---|---|---|
| Definition | Disease caused by pathogenic microorganisms like bacteria, viruses, fungi, or parasites. | Condition or complication caused inadvertently by medical treatment or diagnostic procedures. |
| Cause | Pathogens (e.g., bacteria, viruses). | Medical error, side effects, procedural complications. |
| Transmission | Contagious via contact, airborne, vectors. | Non-contagious; linked to healthcare interventions. |
| Examples | Influenza, Tuberculosis, HIV. | Medication side effects, surgical complications, hospital-acquired infections. |
| Prevention | Vaccination, hygiene, isolation. | Strict clinical protocols, staff training, sterilization. |
| Impact | Public health risk with potential outbreaks. | Patient safety issue within medical care settings. |
Understanding Infectious vs Iatrogenic Diseases
Infectious diseases result from pathogenic microorganisms such as bacteria, viruses, fungi, or parasites invading the body and causing illness, often spread through direct contact, airborne transmission, or contaminated surfaces. Iatrogenic diseases are conditions induced unintentionally by medical treatment or diagnostic procedures, including adverse drug reactions, surgical complications, or hospital-acquired infections. Understanding infectious versus iatrogenic diseases is crucial for accurate diagnosis, appropriate treatment, and improving patient safety by differentiating naturally occurring infections from healthcare-related causes.
Definitions and Key Differences
Infectious conditions result from pathogenic microorganisms such as bacteria, viruses, fungi, or parasites invading the body, causing disease through transmission or contamination. Iatrogenic conditions arise directly from medical interventions, including surgeries, medications, or diagnostic procedures, often as unintended side effects or complications. The key difference lies in the origin: infectious diseases originate from external biological agents, while iatrogenic conditions stem from healthcare activities or treatments.
Common Causes of Infectious Diseases
Infectious diseases primarily result from pathogens such as bacteria, viruses, fungi, and parasites transmitted through various routes including airborne droplets, direct contact, contaminated food and water, or vectors like mosquitoes. Iatrogenic diseases differ, as they stem from medical interventions or treatments, including infections caused by invasive procedures, improper sterilization, or antibiotic misuse. Understanding common causes of infectious diseases, including hygiene lapses and environmental factors, is crucial for effective prevention and control.
Origins of Iatrogenic Conditions
Iatrogenic conditions originate from medical interventions such as surgeries, medications, or diagnostic procedures, often resulting from unintended side effects or errors in treatment. Unlike infectious diseases caused by pathogens like bacteria, viruses, or fungi, iatrogenic conditions stem from healthcare practices rather than external biological agents. Understanding the causes and mechanisms behind iatrogenic symptoms is crucial for improving patient safety and reducing adverse outcomes in clinical settings.
Transmission Pathways: Infectious vs Iatrogenic
Infectious diseases primarily spread through direct contact, airborne particles, bodily fluids, or vectors such as insects, facilitating natural transmission pathways among individuals. Iatrogenic transmission occurs via medical procedures, including contaminated instruments, intravenous lines, or surgical sites, representing a healthcare-associated pathway. Understanding these distinct transmission mechanisms is crucial for implementing targeted infection control strategies and minimizing the risk of healthcare-associated infections.
Clinical Examples: Infectious and Iatrogenic Cases
In clinical settings, infectious cases commonly include bacterial pneumonia, tuberculosis, and viral hepatitis, caused by pathogens transmitting through various routes such as respiratory droplets or blood. Iatrogenic cases arise from medical interventions like catheter-associated urinary tract infections, surgical site infections, and antibiotic-associated Clostridioides difficile colitis, resulting from invasive procedures or medication use. Understanding the distinction aids in prevention strategies targeting microbial transmission and minimizing healthcare-induced complications.
Diagnostic Approaches for Each Category
Infectious diseases require diagnostic approaches such as microbial cultures, polymerase chain reaction (PCR) assays, and serological tests to identify pathogens like bacteria, viruses, fungi, or parasites. Iatrogenic conditions demand careful review of patient history, imaging studies, and laboratory tests to detect complications caused by medical interventions or treatments. Diagnostic precision in infectious cases hinges on pathogen identification, while iatrogenic diagnosis emphasizes correlation with recent medical procedures or pharmaceuticals.
Prevention Strategies: Infection vs Iatrogenesis
Effective prevention strategies for infectious conditions center on sterilization, proper hand hygiene, vaccination, and the use of personal protective equipment to minimize pathogen transmission. In contrast, preventing iatrogenic complications requires rigorous adherence to clinical protocols, accurate diagnostic assessments, cautious use of invasive procedures, and ongoing healthcare professional training to avoid medical errors. Both approaches emphasize risk reduction but target different causative factors: microbial contamination versus procedural or treatment-related harm.
Impact on Patient Outcomes and Healthcare Systems
Infectious complications lead to prolonged hospital stays, increased morbidity, and higher healthcare costs due to the need for extended treatments and infection control measures. Iatrogenic harms, often resulting from medical interventions, can cause adverse patient outcomes including medication errors, surgical complications, and diagnostic delays, significantly impacting trust in healthcare systems. Both infectious and iatrogenic factors strain healthcare resources, emphasizing the importance of robust prevention protocols and continuous quality improvement to enhance patient safety and reduce systemic burdens.
Future Perspectives in Reducing Risks
Emerging technologies in infection control and precision medicine are set to revolutionize the reduction of infectious and iatrogenic risks by enabling targeted interventions and personalized treatment protocols. Advances in genomic sequencing and artificial intelligence facilitate early detection of pathogens and prediction of adverse drug reactions, minimizing complications from medical procedures. Integration of real-time monitoring systems with electronic health records will enhance risk assessment and promote proactive mitigation strategies in healthcare settings.
Infectious Infographic
 libterm.com
libterm.com