Onychomycosis is a common fungal infection that affects the nails, causing discoloration, thickening, and brittleness. This condition can lead to discomfort and may impact your confidence if left untreated. Discover effective treatments and prevention strategies by reading the rest of the article.
Table of Comparison
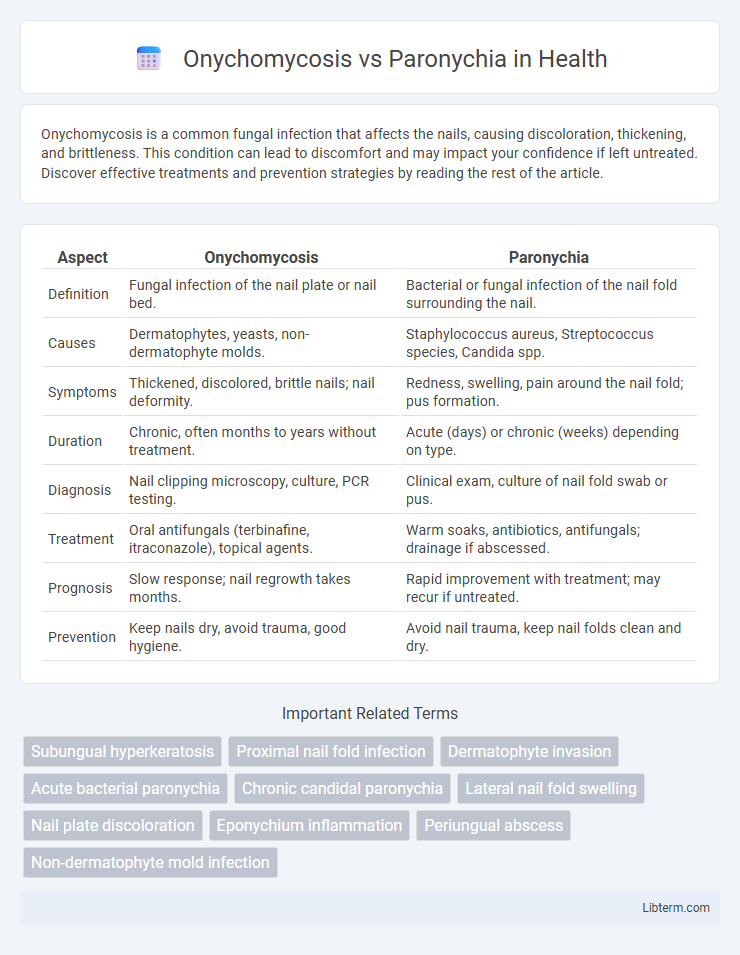
| Aspect | Onychomycosis | Paronychia |
|---|---|---|
| Definition | Fungal infection of the nail plate or nail bed. | Bacterial or fungal infection of the nail fold surrounding the nail. |
| Causes | Dermatophytes, yeasts, non-dermatophyte molds. | Staphylococcus aureus, Streptococcus species, Candida spp. |
| Symptoms | Thickened, discolored, brittle nails; nail deformity. | Redness, swelling, pain around the nail fold; pus formation. |
| Duration | Chronic, often months to years without treatment. | Acute (days) or chronic (weeks) depending on type. |
| Diagnosis | Nail clipping microscopy, culture, PCR testing. | Clinical exam, culture of nail fold swab or pus. |
| Treatment | Oral antifungals (terbinafine, itraconazole), topical agents. | Warm soaks, antibiotics, antifungals; drainage if abscessed. |
| Prognosis | Slow response; nail regrowth takes months. | Rapid improvement with treatment; may recur if untreated. |
| Prevention | Keep nails dry, avoid trauma, good hygiene. | Avoid nail trauma, keep nail folds clean and dry. |
Introduction to Onychomycosis and Paronychia
Onychomycosis is a fungal infection affecting the nails, causing discoloration, thickening, and potential nail deformity. Paronychia is an infection of the nail fold, often bacterial but sometimes fungal, resulting in redness, swelling, and pain around the nail edges. Both conditions impact nail health but differ in their etiology, clinical presentation, and treatment approaches.
Causes and Risk Factors
Onychomycosis is primarily caused by dermatophyte fungi, yeasts, or non-dermatophyte molds infecting the nail plate, often facilitated by prolonged moisture exposure, compromised immunity, or nail trauma. Paronychia results from bacterial infection, commonly Staphylococcus aureus or Streptococcus species, entering through breaks in the skin around the nail, frequently linked to nail biting, manicures, or frequent hand immersion in water. Both conditions share risk factors such as diabetes, peripheral vascular disease, and occupations involving repetitive hand exposure to irritants or moisture.
Clinical Features and Symptoms
Onychomycosis presents with thickened, discolored, brittle nails often accompanied by subungual debris and nail plate distortion, typically affecting toenails more than fingernails. Paronychia manifests as acute or chronic inflammation of the nail fold, characterized by redness, swelling, pain, and sometimes pus formation around the nail margin. While onychomycosis progresses slowly with minimal pain, paronychia usually involves rapid onset of localized tenderness and erythema, often related to bacterial or yeast infection.
Types and Classifications
Onychomycosis is primarily classified into distal lateral subungual, white superficial, proximal subungual, and candidal types, each caused by different fungal pathogens affecting nail structure and appearance. Paronychia is differentiated into acute, typically bacterial in origin with rapid onset, and chronic, often fungal or mixed infection leading to prolonged inflammation around the nail fold. Understanding these classifications aids in targeted treatment strategies and improved clinical outcomes for nail infections.
Diagnostic Approaches
Onychomycosis diagnosis primarily relies on mycological examination, including direct microscopy with potassium hydroxide (KOH) preparation and fungal culture to identify dermatophytes or non-dermatophyte molds. Paronychia diagnosis is mostly clinical, based on the presence of periungual erythema, swelling, and pain, but bacterial cultures and pus aspiration can confirm bacterial etiology, particularly Staphylococcus aureus or Streptococcus species. Dermoscopy and nail biopsy serve as adjunctive tools in differentiating chronic paronychia from fungal infections when clinical presentation is ambiguous.
Treatment Options for Onychomycosis
Effective treatment options for Onychomycosis include topical antifungal agents such as ciclopirox and efinaconazole, and oral antifungals like terbinafine and itraconazole, which have higher cure rates. Laser therapy and photodynamic therapy are emerging alternatives for patients with contraindications to systemic treatments. Proper diagnosis is essential to differentiate Onychomycosis from Paronychia, as the latter typically requires antibacterial or antifungal therapy combined with nail hygiene and sometimes drainage.
Treatment Strategies for Paronychia
Paronychia treatment strategies emphasize prompt management to prevent chronic infection and nail deformities, typically involving warm soaks and topical or systemic antibiotics targeting Staphylococcus aureus and Streptococcus species. In acute bacterial paronychia, incision and drainage are often necessary to eliminate abscess formation. Chronic paronychia requires antifungal therapy combined with avoidance of irritants and moisture to restore the integrity of the nail fold.
Prevention and Self-Care Tips
Onychomycosis prevention includes maintaining dry, clean nails, avoiding prolonged exposure to moisture, and not sharing nail tools, while paronychia prevention focuses on protecting cuticles from trauma, keeping hands dry, and avoiding nail-biting. Self-care for onychomycosis involves regular antifungal treatments and trimming infected nails, whereas paronychia self-care includes warm soaks to reduce inflammation and avoiding irritants. Both conditions benefit from proper nail hygiene and wearing breathable footwear to minimize fungal growth and bacterial infection risks.
Complications and Prognosis
Onychomycosis, a fungal infection of the nails, can lead to complications such as nail thickening, discoloration, and secondary bacterial infections that may result in painful inflammation or permanent nail deformity. Paronychia, an infection of the nail fold often caused by bacteria or fungi, may progress to abscess formation, chronic inflammation, and tissue damage if untreated, sometimes requiring surgical intervention. Prognosis for onychomycosis is typically prolonged due to slow nail growth and potential recurrence, whereas paronychia generally resolves faster with appropriate antibiotic or antifungal therapy but may become chronic in recurrent cases.
Key Differences: Onychomycosis vs Paronychia
Onychomycosis is a fungal infection affecting the nail plate and bed, characterized by thickened, discolored, and brittle nails, primarily caused by dermatophytes such as Trichophyton rubrum. Paronychia is an acute or chronic bacterial or fungal infection of the nail fold, usually presenting with redness, swelling, pain, and sometimes pus around the nail margin. The key difference lies in the infection site and causative agents: onychomycosis targets the nail itself with predominantly fungal etiology, whereas paronychia involves the periungual skin and may result from bacterial or fungal pathogens.
Onychomycosis Infographic
 libterm.com
libterm.com