Melena refers to black, tarry stools caused by the presence of digested blood, typically indicating bleeding in the upper gastrointestinal tract. Recognizing this symptom is crucial for timely diagnosis and management of potential underlying conditions such as ulcers or gastrointestinal cancers. Explore this article to understand the causes, symptoms, and treatment options for melena to safeguard your digestive health.
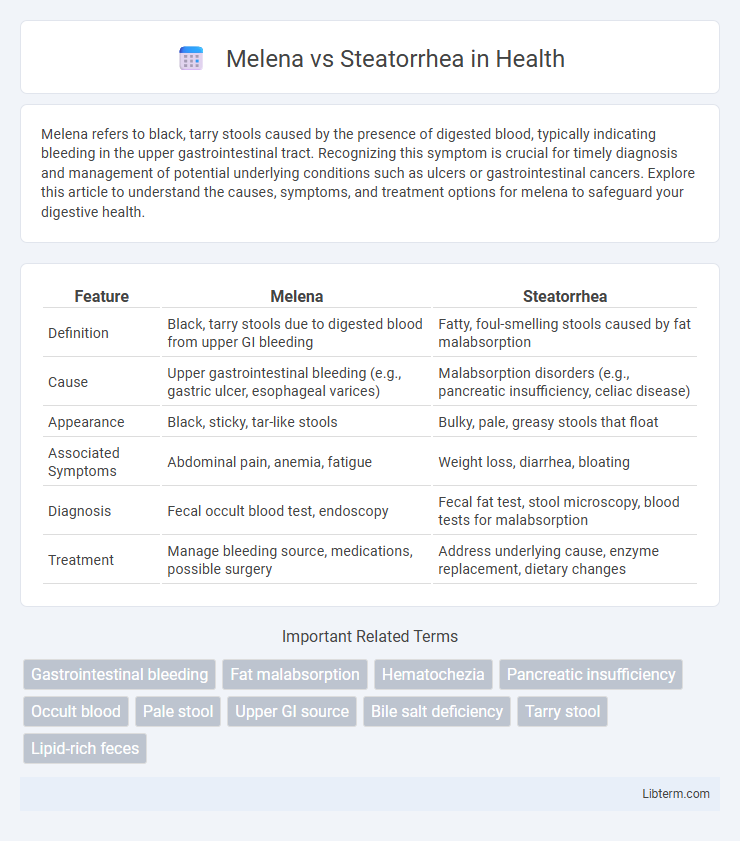
Table of Comparison
| Feature | Melena | Steatorrhea |
|---|---|---|
| Definition | Black, tarry stools due to digested blood from upper GI bleeding | Fatty, foul-smelling stools caused by fat malabsorption |
| Cause | Upper gastrointestinal bleeding (e.g., gastric ulcer, esophageal varices) | Malabsorption disorders (e.g., pancreatic insufficiency, celiac disease) |
| Appearance | Black, sticky, tar-like stools | Bulky, pale, greasy stools that float |
| Associated Symptoms | Abdominal pain, anemia, fatigue | Weight loss, diarrhea, bloating |
| Diagnosis | Fecal occult blood test, endoscopy | Fecal fat test, stool microscopy, blood tests for malabsorption |
| Treatment | Manage bleeding source, medications, possible surgery | Address underlying cause, enzyme replacement, dietary changes |
Introduction to Melena and Steatorrhea
Melena is characterized by black, tarry stools caused by upper gastrointestinal bleeding, often indicating bleeding from the esophagus, stomach, or duodenum. Steatorrhea involves bulky, pale, and foul-smelling stools due to excessive fat content, resulting from malabsorption or pancreatic insufficiency. Both conditions reflect underlying digestive disorders but differ significantly in etiology and stool appearance.
Definition of Melena
Melena is characterized by black, tarry stools resulting from the digestion of blood in the upper gastrointestinal tract, indicating bleeding typically from the esophagus, stomach, or duodenum. In contrast, steatorrhea involves fatty, pale, and foul-smelling stools caused by malabsorption of fats due to pancreatic insufficiency, celiac disease, or bile salt deficiency. Understanding melena's origin as a symptom of upper GI bleeding is crucial for differential diagnosis.
Definition of Steatorrhea
Steatorrhea is the presence of excess fat in stools, resulting in bulky, pale, foul-smelling, and greasy stools that often float due to malabsorption or pancreatic insufficiency. Unlike melena, which indicates upper gastrointestinal bleeding and causes black, tarry stools from digested blood, steatorrhea reflects fat maldigestion or malabsorption. Identifying steatorrhea involves analyzing stool fat content, differentiating it from melena's dark coloration caused by blood degradation.
Causes of Melena
Melena is characterized by black, tarry stools caused by upper gastrointestinal bleeding, typically originating from sources such as gastric ulcers, esophageal varices, or malignancies in the stomach or duodenum. This bleeding leads to the digestion of hemoglobin as blood passes through the intestines, resulting in the distinctive melena color and odor. In contrast, steatorrhea involves fatty, pale stools caused by malabsorption syndromes, pancreatic insufficiency, or bile duct obstructions, without the presence of blood.
Causes of Steatorrhea
Steatorrhea primarily results from malabsorption or maldigestion of fats due to pancreatic insufficiency, celiac disease, or Crohn's disease, leading to excess fat in stool. It can also stem from bile salt deficiency caused by liver or gallbladder disorders, impairing fat emulsification and absorption. Unlike melena, which indicates upper gastrointestinal bleeding, steatorrhea reflects underlying disorders impacting fat digestion and absorption mechanisms.
Key Clinical Differences: Melena vs Steatorrhea
Melena refers to black, tarry stools caused by upper gastrointestinal bleeding, primarily indicating bleeding from sources such as the esophagus, stomach, or duodenum, while steatorrhea involves pale, foul-smelling, bulky stools due to fat malabsorption linked to pancreatic insufficiency, celiac disease, or bile salt deficiencies. Melena is associated with the digestion of blood and presents with symptoms like anemia and fatigue, whereas steatorrhea manifests with weight loss, abdominal cramping, and deficiencies in fat-soluble vitamins (A, D, E, K). Diagnostic approaches differ, with melena identified via stool occult blood testing and endoscopy, while steatorrhea requires stool fat analysis and tests assessing pancreatic function or bile acid metabolism.
Symptoms and Warning Signs
Melena presents with black, tarry stools caused by upper gastrointestinal bleeding, often accompanied by symptoms such as abdominal pain, dizziness, and weakness. Steatorrhea is characterized by pale, bulky, and foul-smelling stools due to malabsorption of fats, frequently linked with weight loss, bloating, and nutrient deficiencies. Warning signs for melena include significant blood loss and anemia, while steatorrhea may indicate chronic digestive disorders like celiac disease or pancreatitis requiring prompt medical evaluation.
Diagnostic Approaches
Melena is diagnosed primarily through stool analysis revealing black, tarry, and foul-smelling stools indicative of upper gastrointestinal bleeding, often confirmed via endoscopy to identify bleeding sources in the esophagus, stomach, or duodenum. Steatorrhea diagnosis involves quantitative fecal fat tests, typically requiring a 72-hour stool collection to measure excessive fat excretion, alongside supportive assessments like pancreatic function tests, imaging studies such as abdominal ultrasound or CT scan, and sometimes small bowel biopsy to evaluate malabsorption causes. Accurate differentiation between melena and steatorrhea relies on correlating clinical presentation with targeted laboratory and imaging diagnostics to guide appropriate therapeutic interventions.
Management and Treatment Options
Management of melena involves stabilizing the patient through fluid resuscitation and blood transfusions if necessary, followed by endoscopic evaluation to identify and treat the source of gastrointestinal bleeding, often employing techniques such as cauterization, clipping, or administration of vasoactive drugs. Steatorrhea treatment focuses on addressing the underlying cause, such as pancreatic enzyme replacement therapy for pancreatic insufficiency, dietary modifications including low-fat meals, and supplementation of fat-soluble vitamins to improve nutrient absorption. Both conditions require tailored interventions based on diagnostic findings, with melena demanding urgent hemostasis and steatorrhea requiring long-term management to restore normal fat digestion and absorption.
Prevention and When to Seek Medical Attention
Prevent melena by avoiding nonsteroidal anti-inflammatory drugs (NSAIDs) and managing conditions like peptic ulcers and esophageal varices through regular medical check-ups. Steatorrhea prevention involves addressing underlying causes such as chronic pancreatitis, celiac disease, or cystic fibrosis with appropriate dietary modifications and enzyme replacement therapy. Seek immediate medical attention if melena is accompanied by dizziness or weakness, or if steatorrhea persists beyond several days with significant weight loss or nutrient deficiencies.
Melena Infographic
 libterm.com
libterm.com