An abscess is a painful, swollen collection of pus caused by a bacterial infection, often occurring under the skin or in other tissues. Proper treatment typically involves drainage and antibiotics to prevent the infection from spreading or worsening. Learn more about symptoms, causes, and effective treatment options in the rest of this article.
Table of Comparison
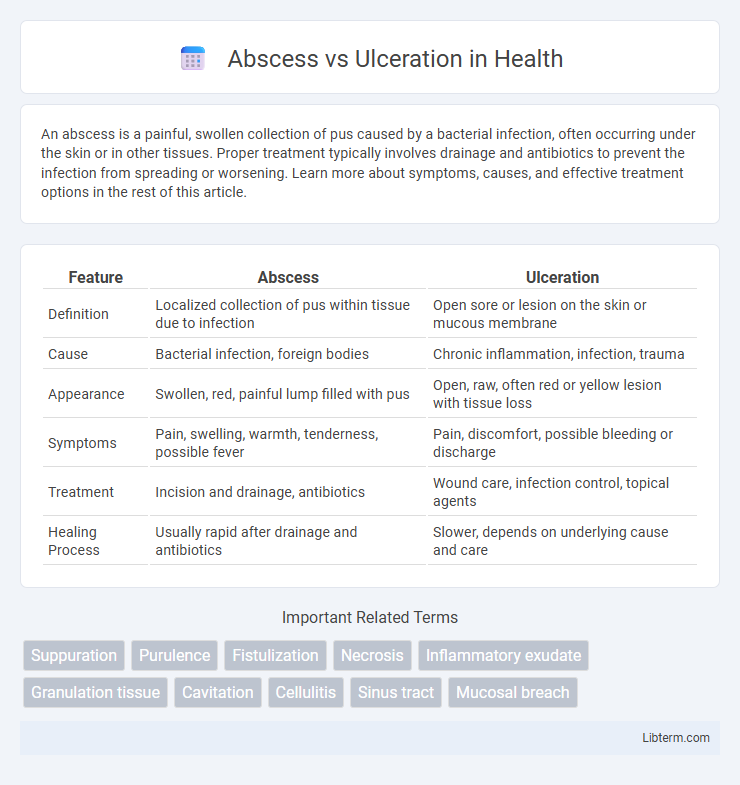
| Feature | Abscess | Ulceration |
|---|---|---|
| Definition | Localized collection of pus within tissue due to infection | Open sore or lesion on the skin or mucous membrane |
| Cause | Bacterial infection, foreign bodies | Chronic inflammation, infection, trauma |
| Appearance | Swollen, red, painful lump filled with pus | Open, raw, often red or yellow lesion with tissue loss |
| Symptoms | Pain, swelling, warmth, tenderness, possible fever | Pain, discomfort, possible bleeding or discharge |
| Treatment | Incision and drainage, antibiotics | Wound care, infection control, topical agents |
| Healing Process | Usually rapid after drainage and antibiotics | Slower, depends on underlying cause and care |
Understanding Abscesses: Definition and Causes
An abscess is a localized collection of pus caused by a bacterial infection, resulting in tissue inflammation and necrosis. It forms when the body's immune response traps invading pathogens, leading to a swollen, painful lump filled with pus. Common causes include bacterial infections from Staphylococcus aureus, trauma, or foreign bodies, which trigger an immune response to contain the infection.
What is Ulceration? Key Characteristics
Ulceration is the breakdown or erosion of the skin or mucous membrane, resulting in an open sore that fails to heal properly. Key characteristics include a visible loss of surface tissue, exposure of underlying layers, and potential presence of inflammation, pain, and discharge. Unlike abscesses, ulcers typically present as open lesions without pus-filled cavities.
Pathogenesis: How Abscesses and Ulcers Form
An abscess forms through localized infection, where bacteria invade tissue, triggering an immune response that leads to pus accumulation and a cavity filled with necrotic debris. Ulceration develops when chronic inflammation or ischemia causes the loss of epithelial tissue, resulting in an open sore that exposes underlying layers. Both conditions involve tissue damage but differ in their pathogenesis, with abscesses characterized by pus-filled cavities and ulcers marked by surface erosion.
Common Sites and Types of Abscesses
Abscesses commonly occur in the skin, oral cavity, and internal organs such as the liver, brain, and lungs, with types including superficial skin abscesses like furuncles and carbuncles, as well as deep-seated abscesses like peritonsillar and intra-abdominal abscesses. Ulcerations primarily affect mucosal and cutaneous surfaces such as the gastrointestinal tract, oral mucosa, and lower extremities, presenting as chronic sores or lesions without pus accumulation. Understanding the distinct anatomical locations and pathological features of abscesses versus ulcerations is critical for accurate diagnosis and targeted treatment.
Typical Locations and Forms of Ulcerations
Abscesses commonly form in soft tissues such as the skin, oral cavity, and internal organs, presenting as localized collections of pus surrounded by inflamed tissue. Ulcerations typically occur in mucous membranes like the gastrointestinal tract, oral mucosa, and genital areas, manifesting as open sores with a necrotic base and irregular edges. Forms of ulcerations include aphthous ulcers, peptic ulcers, and pressure ulcers, each with distinct histopathological features and etiologies.
Clinical Presentation: Abscess vs Ulcer
An abscess presents as a localized, swollen, painful mass often accompanied by redness, warmth, and fluctuance, indicating a pus-filled cavity beneath the skin or mucosa. In contrast, ulceration manifests as an open sore or erosion on the surface of the skin or mucous membrane, typically with irregular edges and a base that may be covered with fibrin or necrotic tissue. Clinical examination differentiates abscesses by palpable induration and possible systemic signs of infection, while ulcers show surface tissue loss without fluctuation.
Diagnostic Approaches: Differentiating Abscesses and Ulcers
Diagnostic approaches for differentiating abscesses and ulcerations primarily involve clinical examination combined with imaging techniques such as ultrasound or MRI to identify the presence of fluid collection characteristic of abscesses versus tissue erosion seen in ulcers. Laboratory tests including cultures and biopsies provide semantic clues by detecting infection markers or histopathological differences, clarifying diagnosis. Employing these diagnostic tools enhances the accuracy of distinguishing between abscesses, which are localized pus-filled infections, and ulcerations, which are tissue surface disruptions often related to chronic inflammation.
Treatment Options for Abscesses
Abscess treatment primarily involves drainage, which can be performed through needle aspiration or surgical incision to remove pus and alleviate pressure. Antibiotics may be prescribed alongside drainage, especially if there is surrounding cellulitis, systemic infection, or immune compromise. Proper wound care and follow-up are essential to ensure complete healing and prevent recurrence or complications.
Management Strategies for Ulcerations
Management strategies for ulcerations involve thorough wound cleaning and debridement to remove necrotic tissue and promote healing, combined with appropriate antibiotic therapy tailored to the infection's etiology. Advanced treatments such as topical growth factors, negative pressure wound therapy, and dressings that maintain a moist wound environment enhance tissue regeneration and reduce healing time. Regular monitoring and controlling underlying conditions, such as diabetes or vascular insufficiency, are critical to prevent recurrence and complications.
Prevention and Prognosis: Abscesses vs Ulcerations
Abscesses require prompt drainage and antibiotic therapy to prevent complications such as sepsis, with prognosis improving significantly when treated early. Ulcerations demand addressing underlying causes like chronic inflammation or vascular insufficiency, and timely wound care to reduce the risk of infection and promote healing. Prevention strategies include maintaining good hygiene, managing chronic conditions, and avoiding trauma to skin or mucosal surfaces for both abscesses and ulcerations.
Abscess Infographic
 libterm.com
libterm.com