Pancreatitis is the inflammation of the pancreas that can cause severe abdominal pain, nausea, and digestive issues. Chronic or acute forms of the condition require timely medical diagnosis and treatment to prevent complications such as pancreatic necrosis or diabetes. Learn more about symptoms, causes, and treatment options to better manage your health in the full article.
Table of Comparison
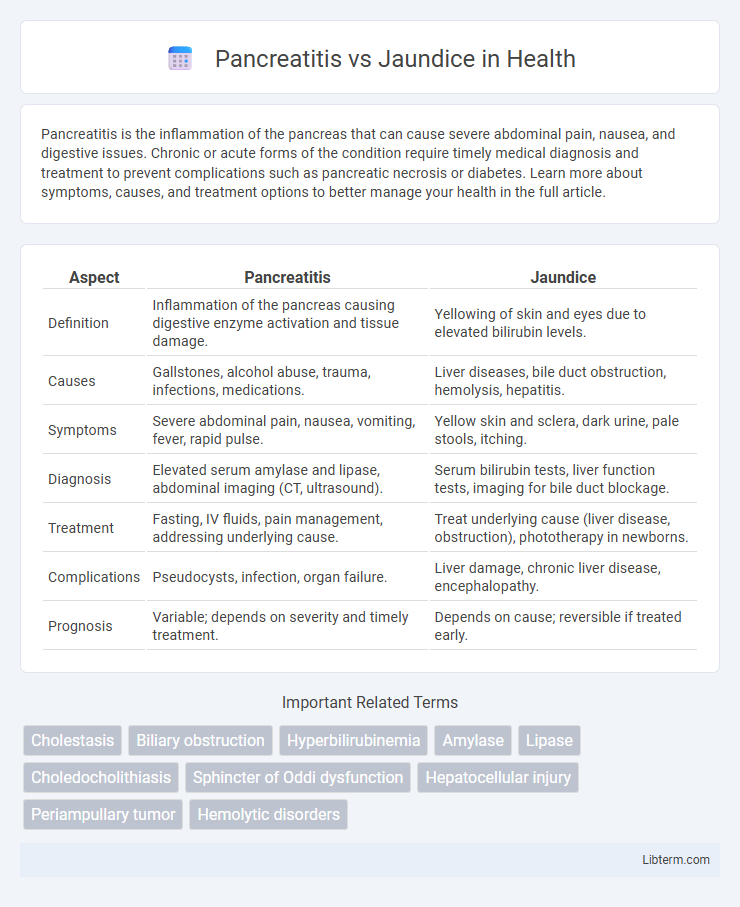
| Aspect | Pancreatitis | Jaundice |
|---|---|---|
| Definition | Inflammation of the pancreas causing digestive enzyme activation and tissue damage. | Yellowing of skin and eyes due to elevated bilirubin levels. |
| Causes | Gallstones, alcohol abuse, trauma, infections, medications. | Liver diseases, bile duct obstruction, hemolysis, hepatitis. |
| Symptoms | Severe abdominal pain, nausea, vomiting, fever, rapid pulse. | Yellow skin and sclera, dark urine, pale stools, itching. |
| Diagnosis | Elevated serum amylase and lipase, abdominal imaging (CT, ultrasound). | Serum bilirubin tests, liver function tests, imaging for bile duct blockage. |
| Treatment | Fasting, IV fluids, pain management, addressing underlying cause. | Treat underlying cause (liver disease, obstruction), phototherapy in newborns. |
| Complications | Pseudocysts, infection, organ failure. | Liver damage, chronic liver disease, encephalopathy. |
| Prognosis | Variable; depends on severity and timely treatment. | Depends on cause; reversible if treated early. |
Understanding Pancreatitis: Causes and Symptoms
Pancreatitis is an inflammatory condition of the pancreas caused primarily by gallstones or chronic alcohol consumption, leading to enzyme activation that damages pancreatic tissue. Key symptoms include severe upper abdominal pain radiating to the back, nausea, vomiting, and elevated pancreatic enzyme levels such as amylase and lipase. Differentiating pancreatitis from jaundice involves recognizing jaundice's hallmark yellowing of the skin and eyes, typically caused by bile duct obstruction or liver dysfunction, rather than pancreatic inflammation.
What Is Jaundice? Overview and Key Indicators
Jaundice is a medical condition characterized by the yellowing of the skin and eyes due to elevated bilirubin levels in the blood, often indicating liver dysfunction or bile duct obstruction. Key indicators of jaundice include dark urine, pale stools, and intense itching, which differentiate it from pancreatitis symptoms like abdominal pain and digestive disturbances. Understanding these signs helps in distinguishing jaundice from pancreatitis and guides appropriate diagnostic and treatment strategies.
Comparing the Origins: Pancreatitis vs Jaundice
Pancreatitis originates from inflammation of the pancreas caused by factors like gallstones, alcohol abuse, or pancreatic duct obstruction, impairing digestive enzyme release. Jaundice results from elevated bilirubin levels due to liver dysfunction, bile duct obstruction, or hemolysis, leading to yellowing of the skin and eyes. While pancreatitis directly affects pancreatic tissue and enzyme activity, jaundice primarily reflects systemic bilirubin metabolism disturbances and liver or bile duct pathology.
Common Risk Factors for Pancreatitis and Jaundice
Pancreatitis and jaundice share common risk factors including excessive alcohol consumption, gallstone disease, and certain infections such as hepatitis. Both conditions are often associated with biliary tract obstruction, which can lead to inflammation in the pancreas and impaired bile flow causing jaundice. Metabolic disorders like hypertriglyceridemia and autoimmune diseases also contribute to the development of pancreatitis and cholestatic jaundice.
Diagnostic Differences: Identifying Each Condition
Pancreatitis diagnosis primarily relies on elevated serum amylase and lipase levels alongside imaging techniques such as abdominal ultrasound or CT scan to detect pancreatic inflammation. Jaundice is diagnosed by elevated bilirubin levels in blood tests and physical examination revealing yellowing of the skin and eyes, with imaging like ultrasound or MRCP used to identify bile duct obstruction or liver abnormalities. Differentiating pancreatitis from jaundice involves assessing distinct biochemical markers and imaging findings: pancreatitis shows pancreatic enzyme elevation and inflammation, while jaundice indicates hyperbilirubinemia with possible biliary or hepatic causes.
Distinctive Symptom Patterns: Pancreatitis vs Jaundice
Pancreatitis typically presents with intense upper abdominal pain radiating to the back, accompanied by nausea and vomiting, while jaundice is characterized by yellowing of the skin and eyes due to elevated bilirubin levels. Pancreatitis symptoms often include abdominal tenderness and elevated pancreatic enzymes such as amylase and lipase, whereas jaundice involves dark urine, pale stools, and itchiness resulting from bile duct obstruction or liver dysfunction. Differentiating these conditions relies on assessing abdominal pain severity and location for pancreatitis, contrasted with the hallmark discoloration and systemic signs seen in jaundice.
Complications Associated with Each Disorder
Pancreatitis can lead to severe complications such as pancreatic necrosis, infection, and acute respiratory distress syndrome (ARDS), with chronic cases increasing the risk of diabetes and malnutrition. Jaundice-related complications often involve underlying liver conditions like cirrhosis or bile duct obstruction, which can cause cholangitis, hepatic encephalopathy, or coagulopathy. Both disorders require prompt diagnosis and management to prevent life-threatening outcomes and organ failure.
Treatment Approaches for Pancreatitis and Jaundice
Treatment approaches for pancreatitis focus on managing inflammation and preventing complications through fasting to rest the pancreas, intravenous fluids for hydration, pain control using analgesics, and addressing underlying causes such as gallstones or alcohol use. Jaundice treatment targets the underlying cause by relieving bile duct obstruction with procedures like endoscopic retrograde cholangiopancreatography (ERCP), managing liver diseases with antiviral or immunosuppressive therapy, and supportive care for symptoms. Both conditions require careful monitoring of liver function tests and imaging studies to guide appropriate interventions.
Prognosis and Recovery: What to Expect
Pancreatitis recovery depends on severity, with mild cases resolving in days and severe cases risking complications like organ failure, impacting long-term prognosis. Jaundice prognosis varies based on underlying cause, ranging from benign bile duct obstruction to serious liver disease, often requiring targeted treatment for full recovery. Both conditions necessitate timely diagnosis and management to improve outcomes and prevent chronic complications.
Prevention Tips and Lifestyle Recommendations
Pancreatitis prevention involves maintaining a low-fat diet, limiting alcohol intake, and avoiding smoking to reduce pancreatic inflammation risk. Jaundice prevention centers on hepatitis vaccination, practicing safe hygiene to avoid liver infections, and regular liver function monitoring for early detection. Both conditions benefit from a balanced diet rich in antioxidants, adequate hydration, and routine medical checkups to support liver and pancreatic health.
Pancreatitis Infographic
 libterm.com
libterm.com